About 5 percent of asthma patients suffer from frequent and severe sudden chest tightness that disrupts breathing, often leading to an emergency room visit and hospitalization.
The condition can best be monitored and treated in a clinical setting, but that’s not where asthma patients live their lives. The challenge is to bring the sophistication of the clinic to asthma sufferers in their everyday lives and activities, because anywhere and anytime is where and when asthma attacks occur.
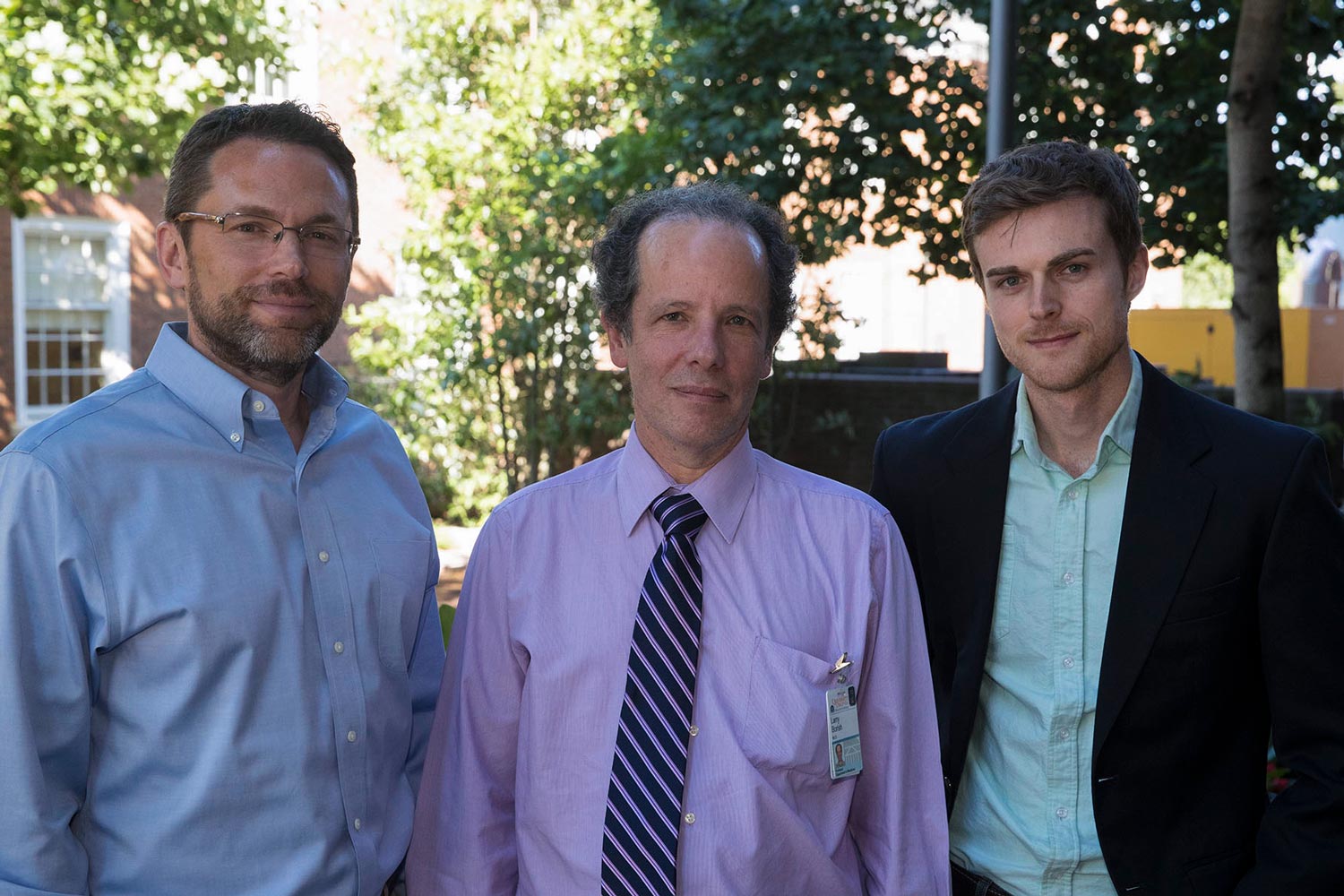
University of Virginia engineering professors Daniel Quinn and John Lach, working with UVA asthma physician Dr. Larry Borish, believe they have found a way to do this. They are developing and testing innovative sensor systems that, once fully designed and implanted in a patient’s trachea, should help detect sudden asthma attacks before they happen, allowing for quick preventive medicative treatment by the sufferer on site, wherever that might be: in the home, on the road, or even on a playing field.
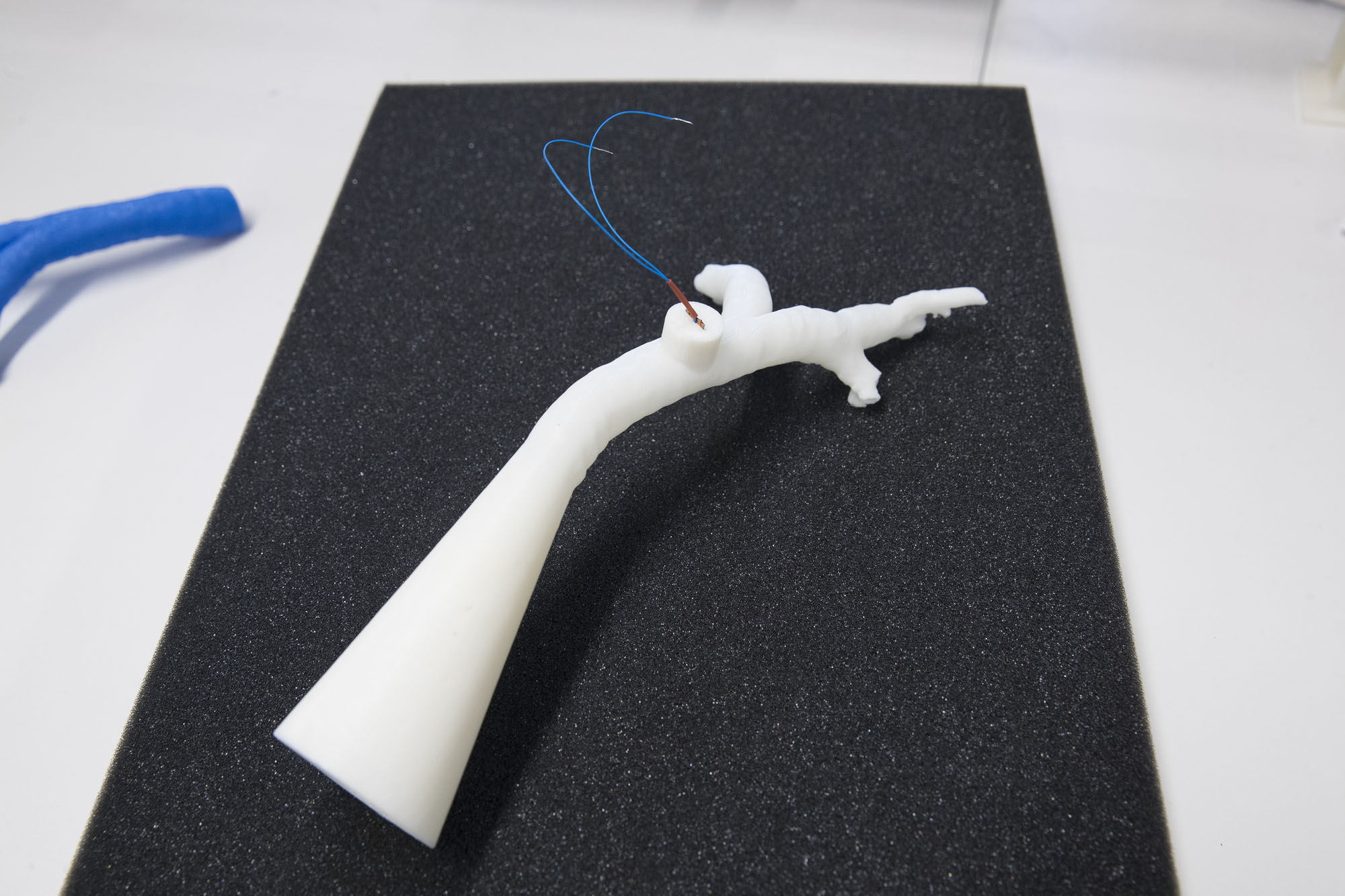
Using 3-D-printed trachea models made to scale, the researchers are testing implantable battery-less sensors that would detect asthma attacks. (Photo by Dan Addison, University Communications)
“Most early detection mechanisms currently available to patients require breathing monitoring in a controlled setting under the supervision of medical professionals using bulky instruments,” said Quinn, a mechanical and aerospace engineer who specializes in fluid dynamics and developing ways to harvest the energy of air flow for anything from air conditioning systems to, in this case, breathing. He described the human trachea as essentially a “scaled-down wind tunnel.”
The UVA team is exploring the feasibility of using a small implanted sensor to internally monitor airflow in people with asthma, while also harvesting the energy from the patient’s breathing to power the sensor without need for batteries, which can fail and periodically need replacement. The technology is innovative in that it would work continuously in the everyday environment. This would be much safer for the patient, less costly, and often would avert the need for trips to the hospital.
Quinn and Lach, who is an electrical engineer, are using tiny devices that include “piezoelectric” materials to generate electricity from tiny motions. Breathing is the energy that would power the implantable mini-air-flow meters that would detect inflammation and obstructions in the trachea and warn of an impending asthma attack.
If this works as expected, the patient would get a warning that an attack is imminent, and would be able to use an inhaler to avert the attack and continue normal activities.
Borish’s expertise with asthma patients provides the clinical understanding of the challenges the engineers face as they develop their system.
“Prior to an asthma attack, very small changes occur in the air flow as the patient breathes,” Quinn said. “We are working to develop sensors that would detect these tiny changes and provide an early warning, even before the patient is aware that the changes are occurring.”
Quinn and Lach work together in the Link Lab at the School of Engineering and Applied Science, a space designed to “link up” researchers from separate disciplines to bring new insights and viable solutions to complex problems from multiple perspectives. And the team, working with Borish, is part of UVA’s new Center for Engineering in Medicine, which brings together engineers and medical doctors and nurses to tackle specific health and health care challenges. The center currently is providing seed funding to 15 multi-disciplinary projects, with more to come.

“This is an exciting and challenging project, and a great way to approach a problem,” Quinn said. “We engineers understand the technologies, and the doctor understands the physiology. We work together to understand each other’s perspective on the problem, and then we use those insights to find solutions. It’s really the next level of engineering.”
The project also includes mechanical and aerospace engineering research scientist Joe Zhu; graduate engineering students Lucy Fitzgerald and Luis Ruiz; and undergraduate engineering students Maria Contreras and Vivian Lin.
“We can enhance insights for new therapies, better medicines and innovative medical devices by bringing creative minds together from across the professions,” said Center for Engineering in Medicine Director Dr. Jeffrey Holmes, a biomedical engineer and medical doctor.
Media Contact
Article Information
September 4, 2018
/content/engineers-physician-collaborating-detect-impending-asthma-attacks