Age is a well-known factor that influences the severity and fatality of COVID-19. In addition, male and female patients are known, at least anecdotally, to fare quite differently in the COVID-19 pandemic. Why might this be, and can these observations help guide potential new treatments? Does gender play a fundamental, causal role in disease severity? If so, is there an age-dependency to the gender parameter?
More broadly, do age, biological sex and any potential gender-related factors (e.g., therapeutic hormone use) somehow interplay in a way that modulates the severity – and ultimate outcome – of a patient’s COVID-19 infection?
Motivated by these questions, Phil Bourne, dean of the University of Virginia’s School of Data Science, and Cam Mura, a senior scientist in the school, are part of an international team that has begun examining these possible interconnections.
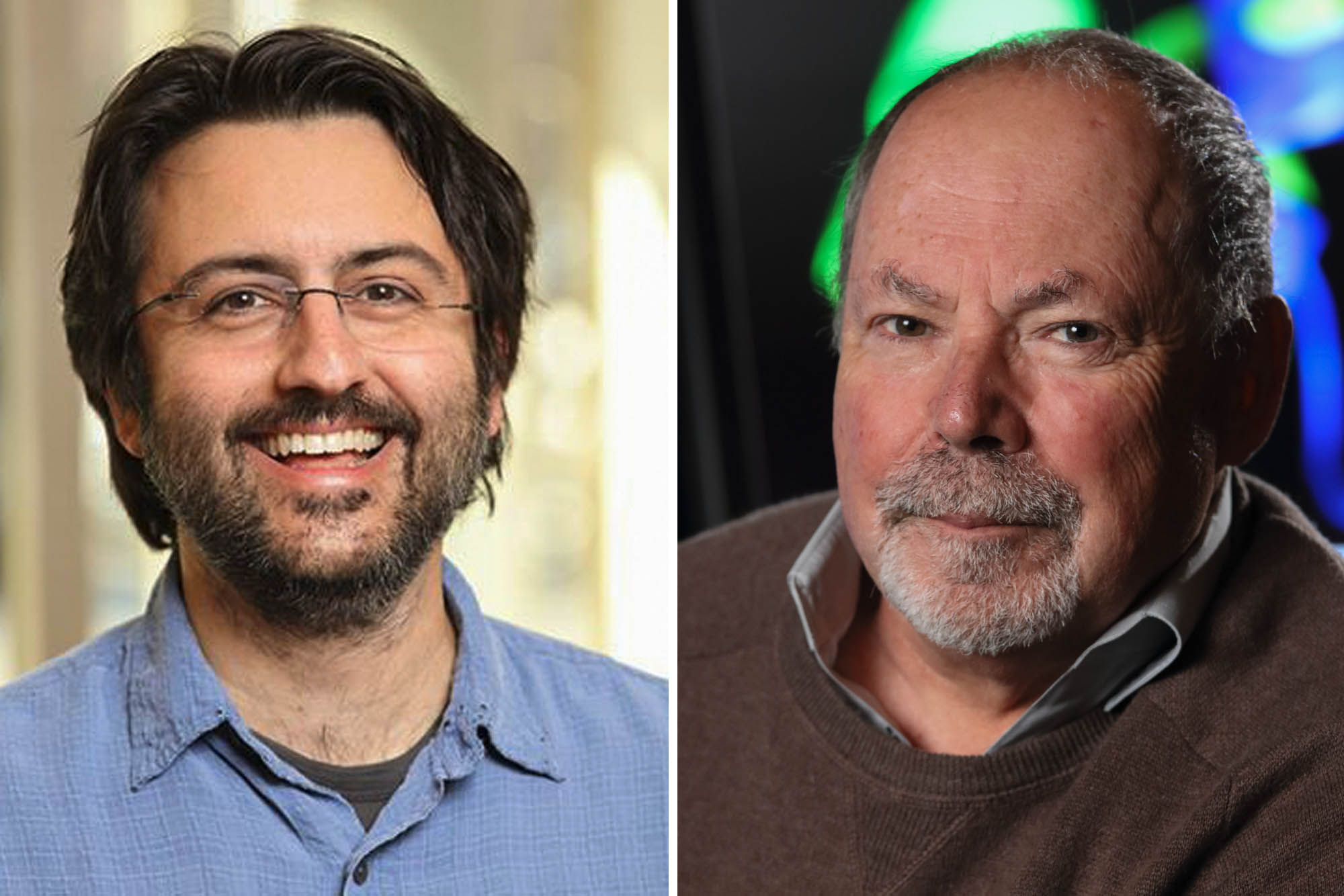
Phil Bourne, right, dean of UVA’s School of Data Science, and Cam Mura, a senior scientist in the school, are part of an international team that analyzed electronic health records of COVID-19 patients. (Photos by Tom Cogill)
In a new project with Dr. Ute Seeland, Robert Preissner and Dr. Saskia Preissner of the Charité–Universitätsmediz in Berlin, and including other collaborators in Germany and Italy, Bourne and Mura have helped analyze electronic health records of nearly 70,000 COVID-19 patients distributed across 17 countries.
By surveying these records, Bourne and Mura found that, indeed, there are statistical trends that track with patient characteristics – chief among these being age, gender and the (age-dependent) usage of estrogen-related hormones (e.g., in post-menopausal women).
“Electronic health records are a treasure trove of hidden discoveries and more digging is needed, something we at the School of Data Science are intent on,” Bourne said.
The three principal findings of the team’s work were: one, in age groups from about 20 to 50 years old, women have moderately higher rates of COVID-19 infection than men; two, in virtually all age ranges, men have higher mortality rates than women, with the effects particularly pronounced beyond age 50 (50% more fatalities among men in their 70s, versus women); and three, among post-menopausal women over the age of 50, use of the hormone estradiol was linked with substantially reduced (by more than 50%) rates of death.
“The latter point, regarding estradiol, is a key factor that underlies and unifies these observed trends: by considering the microscopic, molecular level – the COVID-related immunological and cellular pathways in which estrogen hormones are likely involved – we can elucidate organism-level disease phenomenon,” Mura said.
Bourne added, “These types of studies point to the future of biomedical research: data-driven discovery across scales from molecules to populations – true multi-scale modeling.”
In a nutshell, it’s likely that the apparently protective effects of 17β-estradiol, a naturally occurring, abundant female hormone, relate to a key property of this molecule: it attenuates the so-called “cytokine storm” that’s thought to underlie much of the cellular-scale and organ/tissue-level damage wrought by a SARS-CoV-2 infection, via dysregulation of a patient’s immune response. (SARS-CoV-2, which stands for “severe acute respiratory syndrome, coronavirus 2,” is the technical term for the virus that causes COVID-19.)
Why are men beyond age 50 so much more likely than similarly aged women to suffer from a severe course of COVID-19, including such a greater likelihood of death? Spurred by such questions, and by the possibility of hormone-related therapies, the international research team undertook a detailed examination of electronic health records in light of gender, systematically varying age strata (from 15 years old to age 85-plus), in pre- and post-menopausal patient groups, and in female cohorts that either did or did not use any form of exogenous estrogen-related hormone (e.g., contraception among pre-menopausal adult women, or as part of hormone therapy for post-menopausal cohorts).
Hormone therapy was found to have a strong linkage to the severity and fatality of COVID-19 among women over age 50.
In terms of new therapeutic avenues, Bourne, Mura and colleagues note that “a chief finding of [our] study is the strong positive effect of ... estradiol hormone therapy on the survival rates of post-menopausal women,” and that “whether it could be an effective therapeutic approach not only for women, but also for men with COVID-19 … is a topic for further research.”
The work, published in BMC Medicine, is freely available here.
Media Contact
Article Information
December 3, 2020
/content/age-gender-and-covid-19-complex-hormone-driven-interplay

