Ashton Kutcher revealed this week he has vasculitis, a disease that left the popular actor unable to see, hear or walk for a period.
What is vasculitis, and what is your personal risk?
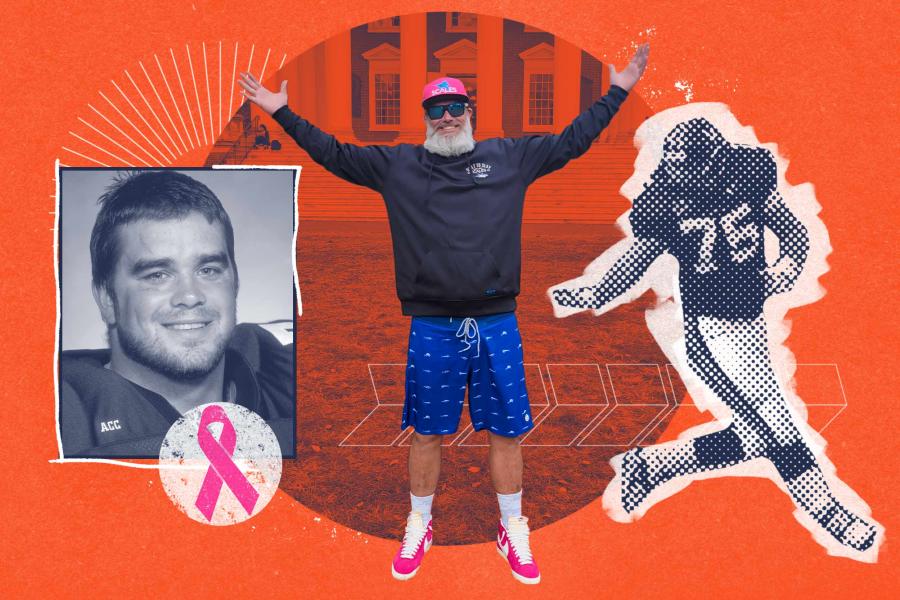
UVA Today spoke to Dr. Randy Ramcharitar, an assistant professor at the University of Virginia School of Medicine and a member of UVA Health’s cardiovascular team. The vasculitis specialist answered questions about the unfamiliar health condition.
Q. What is vasculitis?
A. Vasculitis is inflammation of the blood vessels that can occur anywhere in the body and most often affects the arteries, but can also affect veins. It occurs when our body’s own immune system attacks our blood vessels.
Q. How do you know if you have it?
A. There are many types of vasculitis that can affect arteries of different sizes and different organ systems. This means presenting symptoms can be variable based on the type of vasculitis. Patients can present with rashes, ulcers, limb weakness or pain, kidney and/or lung issues, vision loss, blood clots, stroke or chest pain, to name a few. These are symptoms that can be seen with other medical conditions; therefore, it’s important to be evaluated by a medical provider to help determine the cause.
Q. How common is this disease?
A. Vasculitis is uncommon, but certain types occur more frequently in specific populations. Age, ethnicity and smoking status can increase risk for specific forms of vasculitis.
Q. Can it be fatal?
A. Vasculitis can have significant health consequences for patients, especially if not diagnosed and treated early. In addition to causing inflammation of blood vessels, it can make vessels weaker and prone to aneurysms (enlargement) or dissections (arterial tears). It can also cause arterial stenosis (narrowing) or cause clots in blood vessels. The aneurysms, stenoses, dissections or clots can all decrease blood flow to the limbs and organs such as the eyes, brain or heart, and may lead to death if not properly addressed.