For a medical professional, the questions can be considerably low-tech.
“Can I eat grapefruit?” Dorothy Bishop, 71, asked community health nurse Betsy Peyton, who was kneeling on the floor in Bishop’s living room.
Bishop had heard that eating the acidic fruit might interfere with her medications and Peyton laid it out for her: better to avoid grapefruit because it can hinder the stomach’s natural enzymes and cause too much or too little of her medicines to be absorbed.
Peyton then inquired about Bishop’s foot pain and whether her landlord had taken care of a mildew issue in her apartment.
The questions were all part of a home visit with Bishop, one of about 60 clients who Peyton and two other community health workers regularly see across Central Virginia. The visits are part of WellAWARE, a program that acts like the proverbial connective tissue between high-tech medicine and clients’ often low-tech, high-touch needs, like grapefruit guidance.
The program focuses on people who frequently use local emergency rooms for low-acuity health problems while avoiding preventative primary care.
“Maybe you’re not hanging an IV like you’d do in a hospital,” said Peyton, the pilot program’s founder and a double Hoo who returned for her bachelor’s degree in nursing, “but you’re talking about some really important stuff.”
Just shy of its three-year anniversary, WellAWARE’s results speak volumes. Clients with the organization for at least six months use the emergency room 48% less often and are hospitalized 30% less frequently.
Peyton, who hopes to secure funding to continue and expand the program, sees its value to humans and hospitals’ bottom lines in real time.
I’ve always appreciated the therapeutic value of listening to people’s stories.
WellAWARE’s three staffers are professional problem-solvers who help clients overcome entrenched barriers to good health and health care. They organize medications. They offer nutrition counseling. They purchase air conditioning units and intervene with difficult landlords. They give rides to food banks and pharmacies, pass out gas and grocery cards, figure out what to do if the electricity or water’s been cut off, and even handle a snake in the house.
Zeroing in on those who might fall through the cracks, WellAWARE’s help is grassroots and person-to-person.
As a student at UVA, Peyton was inspired to pay special attention to the patients who sometimes got overlooked. After becoming a nurse, Peyton worked in group homes, with dementia patients, on a locked psychiatry unit, and found a passion for being with people when they’re “not at their best.”
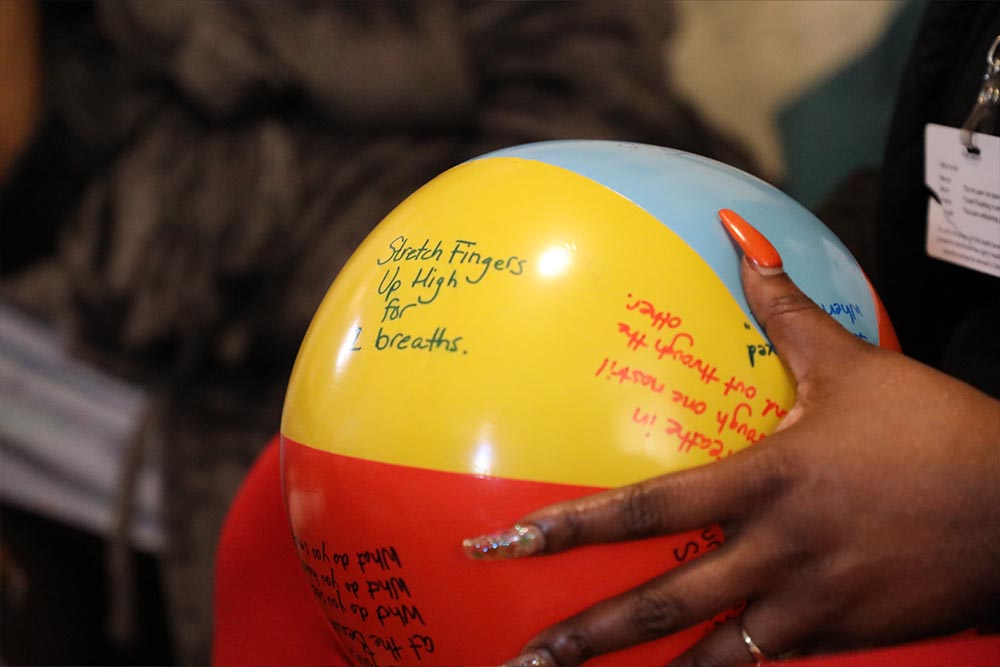
WellAWARE’s staffers take care of patients in all kinds of ways, from organizing medications to giving out gas cards. (Photo by Christine Kueter, UVA School of Nursing)
“I really respect the dignity of people when they’re struggling,” Peyton said. “Psychiatric nursing is a field where you’re often called just to be with people and hear their stories. I’ve always appreciated the therapeutic value of listening to people’s stories.”
For the first nine months of 2021, Peyton knocked on doors, chatted on porches, attended neighborhood association meetings, and tuned in. Guided by census-tract maps showing areas where citizens frequently turned to emergency rooms for primary care, Peyton’s approach built trust and gave community members a sense of ownership in the project.
Begun as a collaboration with the Charlottesville Free Clinic, UVA Primary Care and Central Virginia Health Services, WellAWARE offers help that augments the groups’ services and the clients’ needs. Peyton and her colleagues do house calls – the kind of care that she was drawn to, and which has been demonstrated to save money.
“When the health care system saves money, it’s good for everyone across the board. But that’s not what I wake up most excited about,” Peyton said. “It’s the benefits to the community, to our neighbors, to local families and individuals that makes this work so worthwhile. It really works.”






