The University of Virginia collaborated on research, released Wednesday, that found commercially available COVID-19 vaccines could be more effective against new variants if paired with a type of messenger RNA vaccine now in development.
In about 100 hamsters, the researchers found the combination “induced more robust control of the delta and omicron variants in the lungs, but also provided enhanced protection in the upper respiratory tract,” the study reports. The findings were published in the journal Science Translational Medicine.
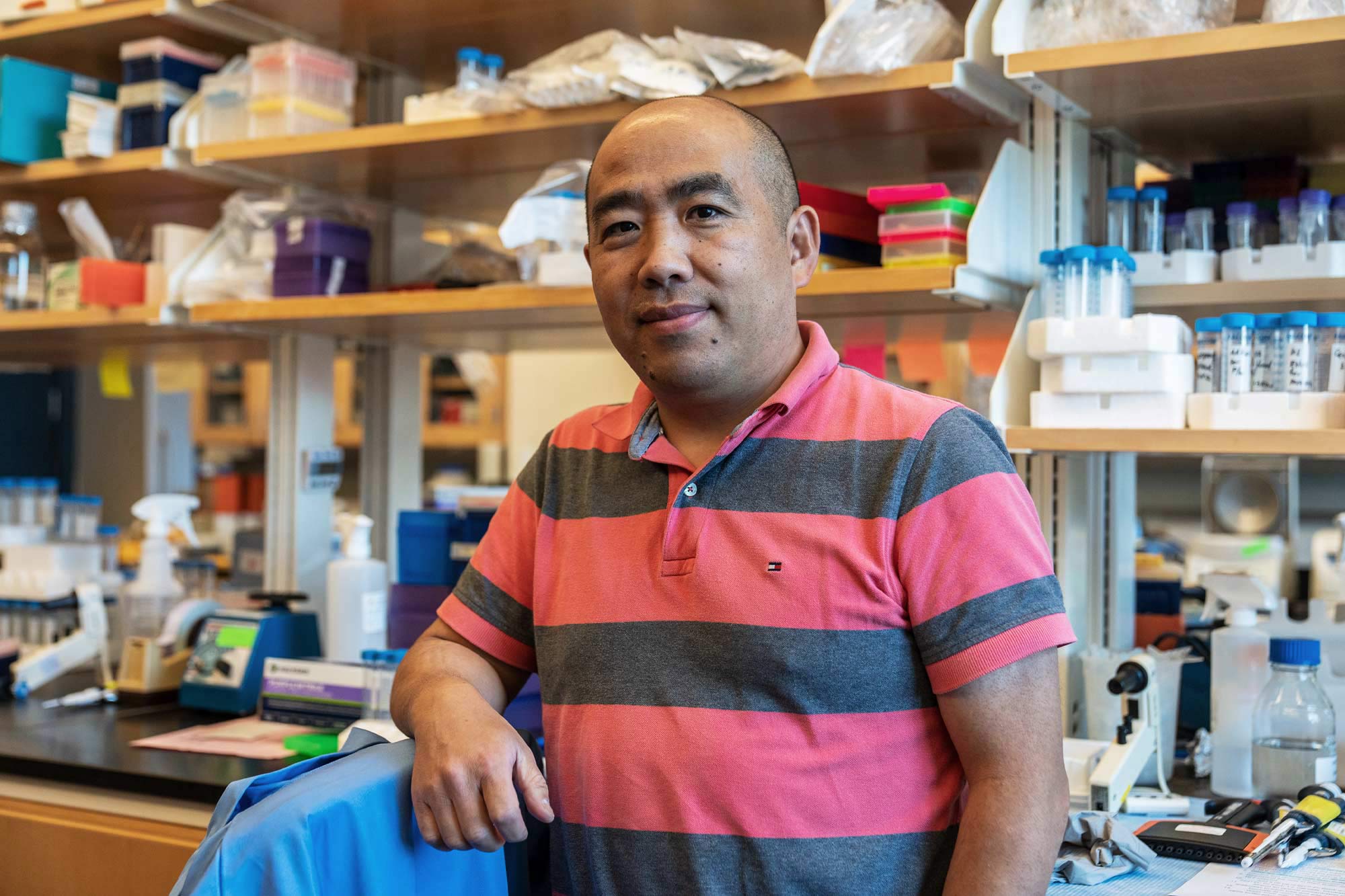
Although testing of the combination has not yet progressed to human trials, the relatively high protective immunity focused in the lungs shows great promise, said Jie Sun, Harrison Distinguished Teaching Professor of Medicine at UVA.
Specifically, research led by the University of Texas combined a vaccine that targets the spikes on the surface of the coronavirus – the kind of mRNA vaccine most of us have received by now – with a less familiar type that targets the virus’ nucleocapsid. That’s the surrounding protein that coats the virus’ nucleic acid. Researchers often refer to the separate proteins by their first letters – “S” and “N” – for short.