Targeted temperature management – the precise cooling of a person suffering cardiac arrest – can literally be the difference between life and death. Now researchers at the University of Virginia and the Cleveland Clinic have developed a new tool to predict how much the treatment will benefit a patient. They hope the new tool will be both helpful and a comfort to patients’ families, particularly when they must make difficult care decisions.
“There is a period of time where you can’t really evaluate a patient very well in terms of whether they are likely to survive … and that’s, of course, what everybody wants to know,” said Dr. Lawrence W. Gimple of the UVA Health System. “It’s important to realize that you don’t know, you can’t know. So what we developed was a model to help you to predict the probability that someone will get better.”
Targeted Temperature Management
Targeted temperature management is a relatively recent innovation and is offered at leading-edge hospitals such as UVA. When a patient arrives after suffering cardiac arrest – as a result of coronary artery disease, for example, or a heart attack – doctors lower the patient’s temperature significantly, typically to somewhere between 91.4 and 93.2 degrees. This improves both survival and brain function upon recovery.
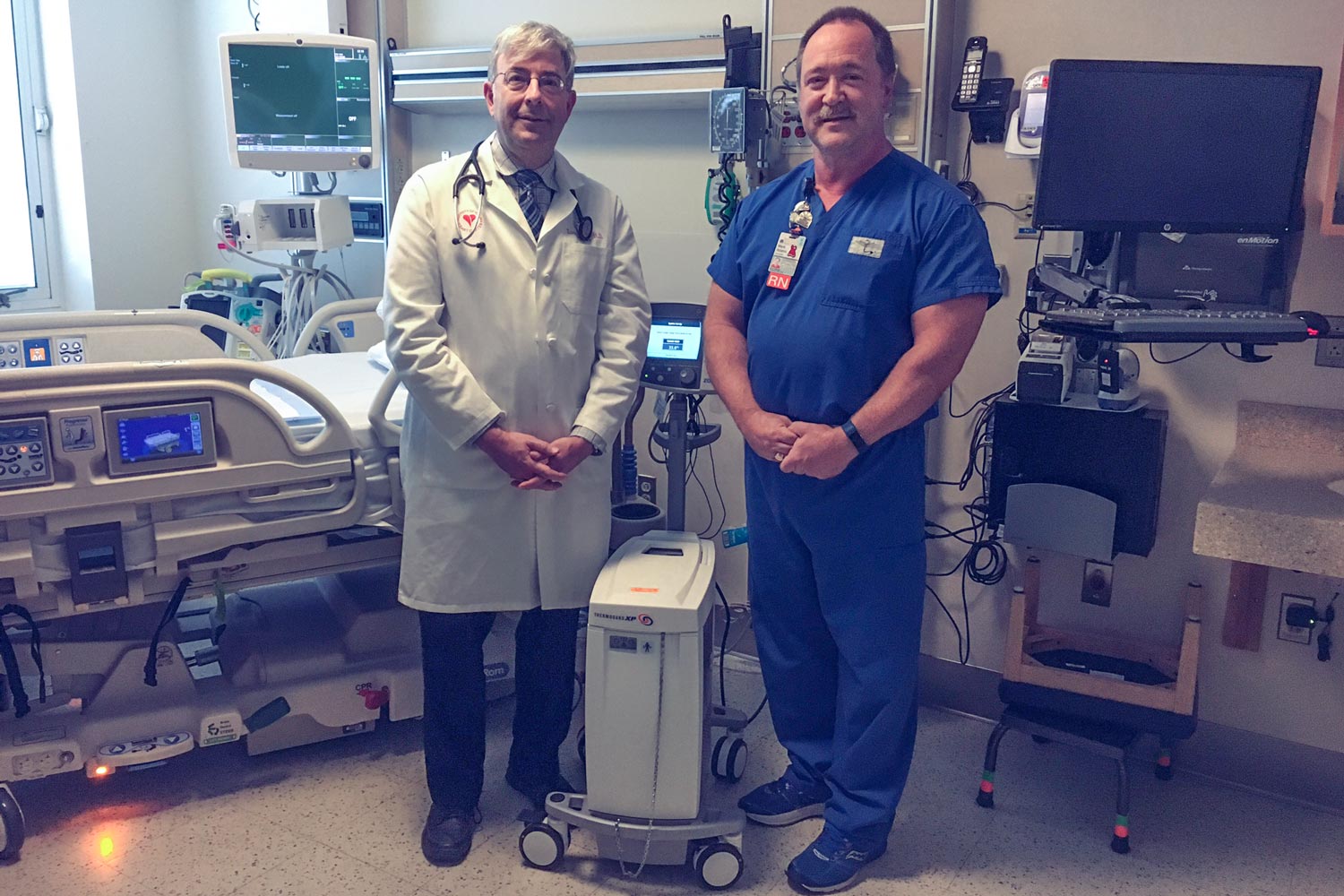
Dr. Lawrence W. Gimple, left, and Mark Adams, nurse manager of UVA's Coronary Care Unit, were among the researchers who developed the model.
After lowering the body temperature, there is a period of uncertainty about the patient’s prognosis. It’s hard to tell if the person will survive, and, if so, if he or she will have meaningful neurological function. That’s where the new tool, developed by Gimple and colleagues at UVA and Cleveland Clinic, comes in.
Called C-GRApH, the tool looks at facts available when the patient is admitted to the hospital, including the patient’s age, blood pH reading, glucose level, the initial heart rhythm and presence of coronary artery disease, to calculate a score from 0 to 5. The lower the score, the more favorable the prognosis, and the more likely the patient will recover with substantial cognitive function.
Cardiac Arrest Outcomes
Gimple, UVA’s director of clinical cardiology, emphasized that doctors would never make treatment decisions based solely on the predicted outcome. That, he said, is just one data point among others to be considered. But a prediction that a person has a significance chance of recovering can be comforting news to a family in distress, he noted. Even a prediction that a patient will not recover might be a comfort, he said, to a family making difficult choices about end-of-life care. “All of the predictions are based on scores that could give doctors and families greater perspective,” Gimple said.

Findings Published
The researchers have described the new method in an article published in the Journal of the American Heart Association. The team included Dr. Erich L. Kiehl, Dr. Alex M. Parker, Dr. Ralph M. Matar, Dr. Matthew F. Gottbrecht, Dr. Michelle C. Johansen, Mark P. Adams, Lori A. Griffiths, Steven P. Dunn, Katherine L. Bidwell, Dr. Venu Menon, Dr. Kyle B. Enfield and Gimple.
Media Contact
Article Information
August 25, 2017
/content/cool-tool-innovation-predicts-patients-outcomes-after-cardiac-arrest

