Find the latest information on the University’s response to the coronavirus here.
University of Virginia history professor Christian W. McMillen literally wrote the book on pandemics.
The author of “Discovering Tuberculosis: A Global History, 1900 to the Present” and “Pandemics: A Very Short Introduction,” McMillen researches the history of epidemic disease, as well as American Indian history.
A member of the Corcoran Department of History since 2004, McMillen is also associate dean for the social sciences in the College of Arts & Sciences and a member of UVA’s Global Infectious Diseases Institute. His focus on medical history had generated his course “Epidemics, Pandemics and History,” which is also featured in the University’s Global Studies program. He has lectured on pandemics and epidemics at the School of Medicine.
McMillen recently took the time to answer a few questions about how the COVID-19 pandemic compares with some of the pandemics of the past.
Q. What is the difference between an “epidemic” and a “pandemic?”
A. Epidemiologists might have different ways of seeing an epidemic and a pandemic than I do as a historian. A pandemic has a formal definition, but in a basic way, a pandemic is just a really big epidemic; it travels across vaster amounts of time and space.
Q. How does the novel coronavirus pandemic compare to the pandemics you researched for your books? What, if anything, is different from previous events?
A. The clearest historical analogies are cholera in the 19th century, the 1918 influenza and, without wanting to seem too alarmist, the Black Death, which signaled the arrival of the second plague pandemic in Europe in 1347. Both the plague and cholera were new and unknown; neither were treatable. They both came on very quickly.
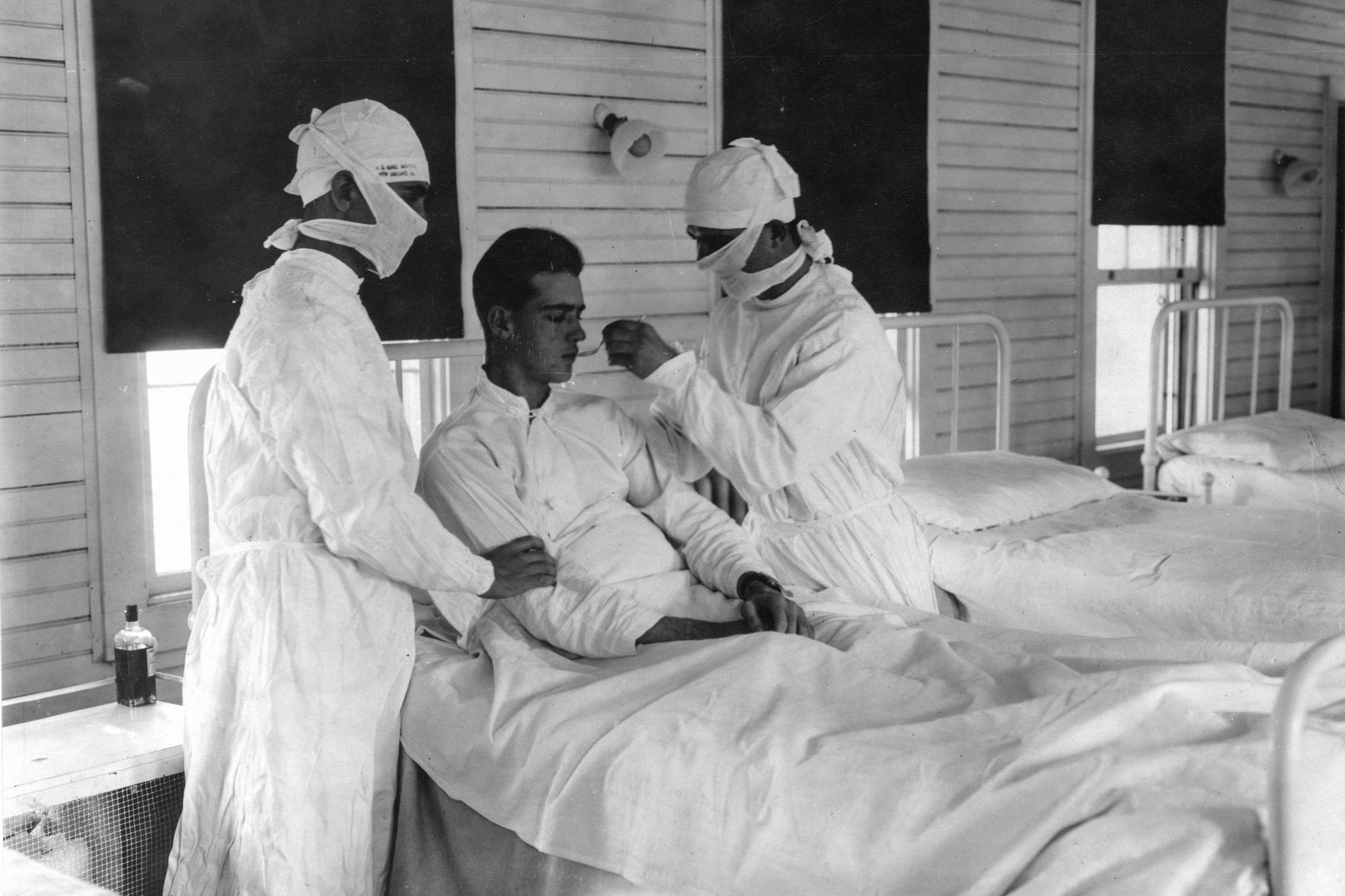
In 1918 the flu pandemic that emerged in the spring of 1918, then really got bad in the fall of 1918, was initially thought not to be terribly serious by many. There had been annual flu epidemics. It is analogous to our experience with COVID-19 because you see similar patterns emerging of initially not taking it seriously, initially saying this is no worse than the normal seasonal flu.
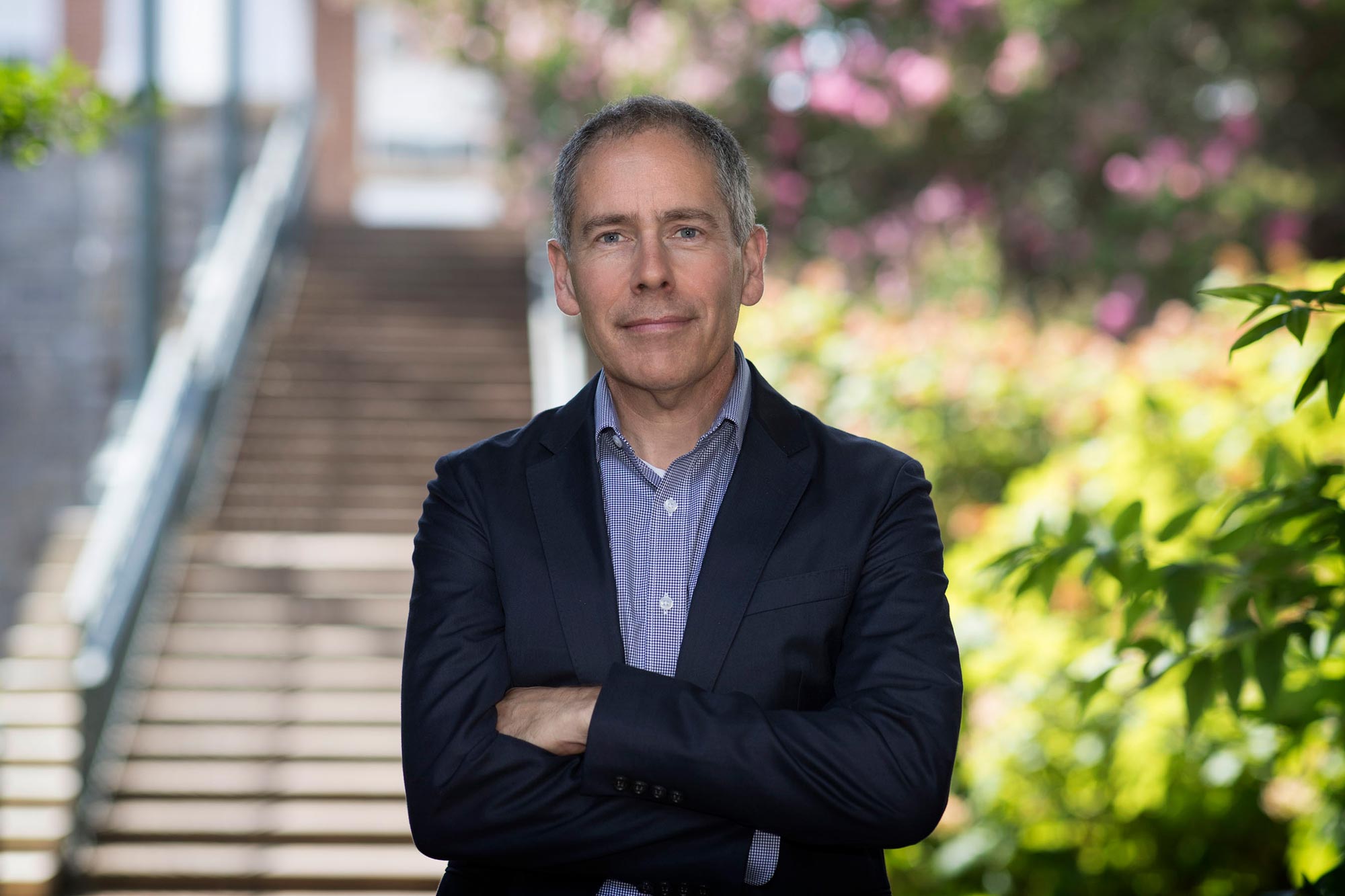
Historian Christian W. McMillen literally wrote the book on pandemics. (Photo by Dan Addison, University Communications)
Q. How is this one different?
A. It is different because it is a novel coronavirus, a different disease. If cholera arrived in an epidemic or pandemic form now, we would know what to do about it; whether we would or not is a different question.
In the case of coronavirus, we don’t really know what to do about it. The plague, cholera and the flu all travel throughout the world in exactly the same way the coronavirus is traveling through the world now; it just happens faster. I think a fundamental difference is that it is arriving in a world that has a greater population and news can travel that much faster. We live in a time of misinformation and distrusted information. But this applies to other eras too. There was much misinformation about cholera and influenza, too, but the scale is different.
Q. What about more recent episodes such as SARS, swine flu, the avian flu and Zika virus?
A. The difference in each of those cases – and I don’t want to overstep my expertise as a historian – but the contagiousness in each of these cases is different. So was their severity. In the case of coronavirus, it seems quite contagious. It is relatively easy to get. We squandered four to six weeks not preparing to do anything about it. Zika and Ebola are harder to transmit than coronavirus.
Q. Is there a way to predict and/or prepare for pandemics?
A. Yes. In terms of prediction, we always know another one is coming; by this point in human history, we should not be surprised.
In terms of preparing, don’t dismantle the public health infrastructure around the world, don’t dismantle the White House’s National Security Council Directorate for Global Health Security and Biodefense, don’t cut funding to the Centers for Disease Control.
Q. How do pandemics shape history? What are some specific examples?
A. They can have demographic effects, like the 1918 flu seems to have had on India, where mortality was higher among women than men and the birthrate appears to have fallen in the year after the pandemic killed between 12 to 18 million people. They present an opportunity to do critical research on the ways diseases travel through populations. They force people to develop medical interventions that otherwise might not have been developed. They can thus be boons to our understanding of disease and boons to medical research.
That is a tragic irony. The plague and cholera, in part, drove the creation of a public health infrastructure and in developing states’ capacities to respond to public health crises. The HIV/AIDS pandemic launched a global health activist movement around equal access to medicine. The list goes on.
Q. Any examples of how pandemics changed populations?
A. All historical events are always about change. Cholera changed the way the medical profession understood how diseases were transmitted, and changed the way medical personnel understood the contagious nature of disease.
For a very long time, medical doctors thought diseases such as cholera were transmitted through the air. They were products of the local environment; if you mitigated the local environment, you would be able to stop cholera. But over the course of the 19th century, that notion changed as people came to understand that cholera was a single organism that was transmitted through contaminated water. And this led to a new understanding of how diseases were transmitted and how people got disease.
Q. From your perspective as a historian, can you predict what lasting societal changes the coronavirus pandemic might cause?
A. Historians are really pretty cautious about this sort of thing, but I can imagine that if the government responds in a robust and sustained way, it will make people understand that having a government that is able to act in the best interests of the entire citizenry is good.
The government is not the enemy of the people. People are looking to President Franklin Roosevelt’s response to the Great Depression as an example of how a government and a president can respond to a national crisis. It is possible that there is an opportunity to do that now, to respond actively and robustly in a sustained way that would reinvigorate people’s faith and trust in government.
Q. Do you have any advice for our readers whose lives have changed abruptly in the past week because of this pandemic?
A. I would say that the worst thing people can do is to become complacent and allow governments and businesses to lose focus and become complacent as well. It is really clear, in the late 19th century in England and elsewhere in Europe, that as smallpox began to taper off in the population, people became complacent about vaccination. As a result, the incidence of smallpox began to rise all across Europe. Complacency, in this case, was fatal.
In the case of the 1918 flu, some American cities started relaxing their quarantine and social distancing measures too soon and the disease surged again. I think as frustrating as it will be, there are enough historical examples of complacency and thinking we have solved the problem too soon and then the disease surging again. So I think people should be prepared for dealing with this for a considerable period of time and to not give in too soon.
Media Contact
Article Information
March 23, 2020
/content/qa-how-does-covid-19-stack-pandemics-past