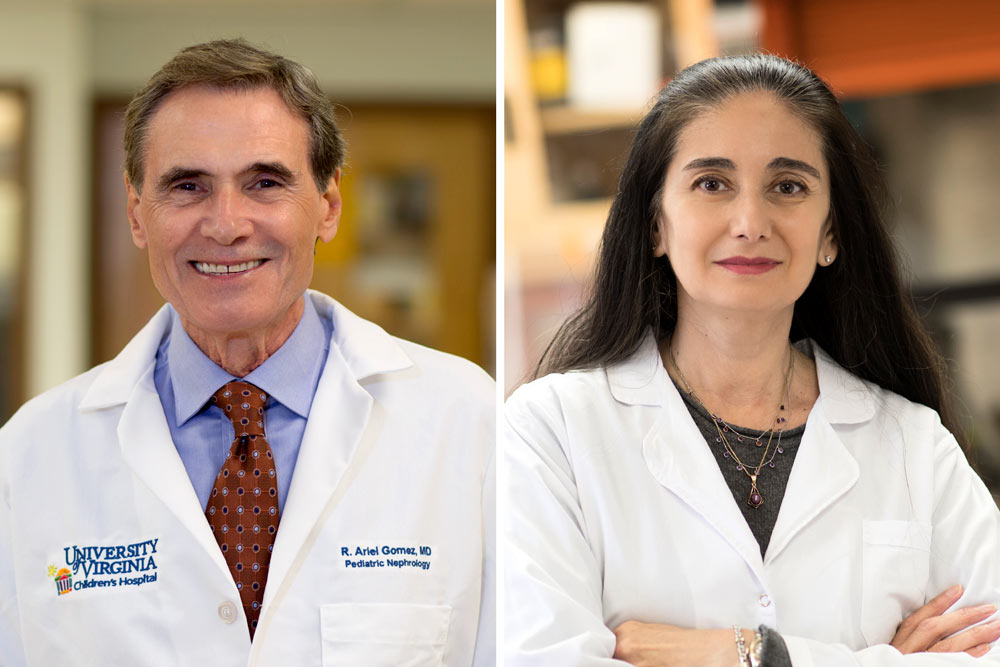
“Discovering how the switch works will help us understand how our bodies control blood pressure,” said researcher Dr. R. Ariel Gomez of UVA’s Child Health Research Center. “Knowing how vascular cells change their identity could help develop new medications to treat high blood pressure and vascular diseases.”
Understanding Blood Pressure
Gomez and his collaborator, Dr. Maria Luisa S. Sequeira-Lopez, are leading researchers into the role of renin in blood pressure control. They worked with UVA senior scientist Jason P. Smith and collaborators to better understand how the cells suddenly remember how to make renin long after they have stopped doing so.
The UVA team identified several biological mechanisms, including nine genes that play key roles in three biological pathways that regulate renin production, controlling when smooth muscle cells stop producing renin and when they start again.
The scientists noted that while such cells stop producing renin naturally, they remain “poised” to reactivate when necessary. They also discovered factors that trigger the genes to resume renin production. This “epigenetic” switch is the lynchpin to understanding how renin production is controlled in those cells that don’t normally produce renin.
“We expected to find the region in your genome where this gene is located to be inaccessible when renin is turned off, but it turns out this spot stays generally accessible in cells ready to be called into action when more renin is needed,” Smith said.
“Ultimately, since renin is so critical for our own health, a better understanding of how our bodies control its production may prove foundational to how we treat hypertension (high blood pressure) and the long-term effects of common blood pressure medications on kidney function and disease.”
The findings offer guidance for future research and could provide important insight into the progression of dangerous kidney damage called fibrosis. The researchers suggest targeting the renin-control processes could lead to new treatments for high blood pressure and cardiovascular disease.
“Now we want to identify markers and potential targets to mitigate and hopefully control unwanted effects of chronic stimulation of the renin cells,” Sequeira-Lopez said. “It is crucial to understand the basic secrets of our cells to design more and more effective therapies with less or no adverse effects.”