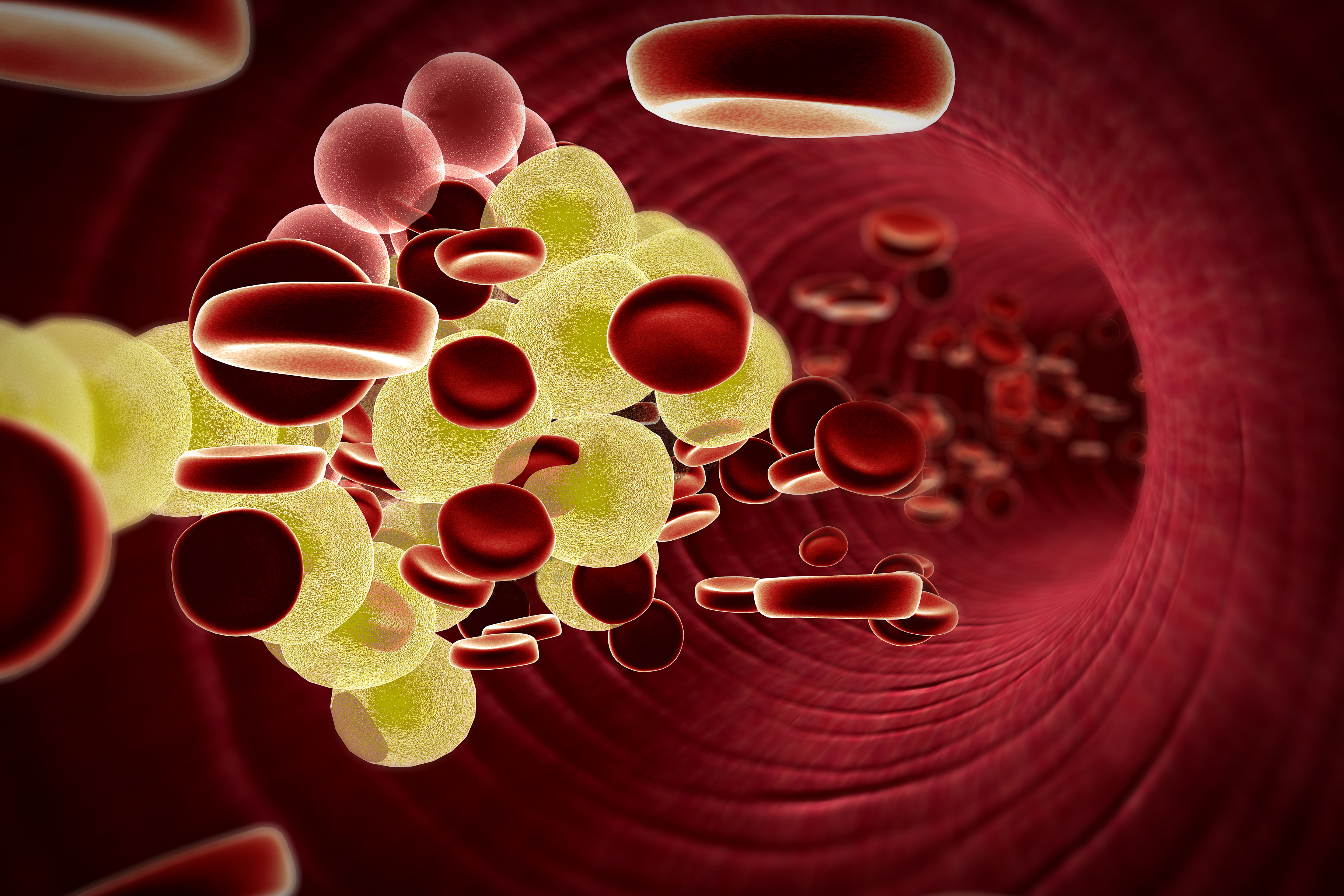
A discovery about how the body deals with the cholesterol contained within its dying cells has suggested an exciting new approach to control people’s cholesterol levels – and thus their risk of developing heart disease.
The discovery from the School of Medicine reveals a previously unknown mechanism by which cells that are about to die inform the cells that are about to eat them how to handle the cholesterol they contain. By stimulating or simulating this molecular messaging, doctors may one day be able to better regulate the body’s levels of HDL and LDL cholesterol – the so-called “good” and “bad” cholesterols.
“We turn over roughly a million cells in the body per second as part of routine, healthy living, and these ‘corpses’ are rapidly eaten and processed by neighboring cells referred to as phagocytes,” researcher Kodi S. Ravichandran said. “But there’s a challenge here: When a phagocyte eats another cell, it’s basically like your neighbor moving in with you with all their belongings. The phagocyte that has just eaten the dying cell has to manage all the cholesterol, lipids, proteins, carbohydrates and other components that have come from the target it has just eaten – on top of maintaining its own routine metabolism.”
The discovery made by Aaron Fond, a graduate student in Ravichandran’s laboratory, explains how the dying cells offer one type of deathbed instructions for dealing with their excess cholesterol. That knowledge opens the door to targeted therapies that could control the process, using a more physiological trigger than existing methods.

UVA researcher Kodi S. Ravichandran and his team have identified a new mechanism that has the potential to be manipulated to regulate cholesterol levels.
The discovery in Ravichandran’s laboratory offers a way to stimulate cholesterol transport and removal as the body does naturally: through cellular messaging. “When we were studying how phagocytes that ingest apoptotic [dying] cells regulate cholesterol, what we discovered was that the dying cells use a completely novel mechanism,” he said. “Dying cells expose certain membrane lipids or so called ‘eat-me’ signals on their surface. When these are recognized by phagocytes via specific receptors, this triggers a pathway [in the phagocytes] that ultimately leads to [an increase in] the levels of a very important cholesterol transporter, ABCA1.”
This is a process that appears to be completely independent of the LXR pathway now being targeted. Importantly, many human studies have shown an association between ABCA1 levels and cardiovascular disease.
Fond, Chang Sup Lee, Ravichandran and colleagues have now discovered the components of the molecular machinery by which dying cells boost ABCA1 in phagocytes. They discovered that when the phagocytic receptor BAI1 engages the dying cell, this initiates a signal to increase ABCA1. Mice lacking BAI1 had a worse HDL/LDL ratio, while mice that express more BAI1 showed a beneficial effect.
“In mice with greater levels of this receptor BAI1, not only do the phagocytes eat better, they up-regulate ABCA1 and show an improved ratio of HDL versus LDL cholesterol,” Ravichandran said.
Ravichandran, who chairs UVA’s Department of Microbiology, Immunology, and Cancer Biology, is working on potential ways to prompt this effect in humans.
“We have the opportunity now to target this BAI1 receptor and/or signaling via this pathway directly,” he said. “This would, in turn, have a beneficial role in regulating cholesterol and help prevent the damaging cardiovascular effects.”
The discovery has been described in the Journal of Clinical Investigation. The paper’s authors are Fond, Lee, Ira G. Shulman, Robert S. Kiss and Ravichandran.
Media Contact
Article Information
November 19, 2015
/content/dying-cells-uva-finds-potential-way-control-cholesterol-levels