University of Virginia School of Medicine researchers have identified a potential treatment for the respiratory symptoms of long COVID after discovering a previously unknown cause of the condition inside the lungs.
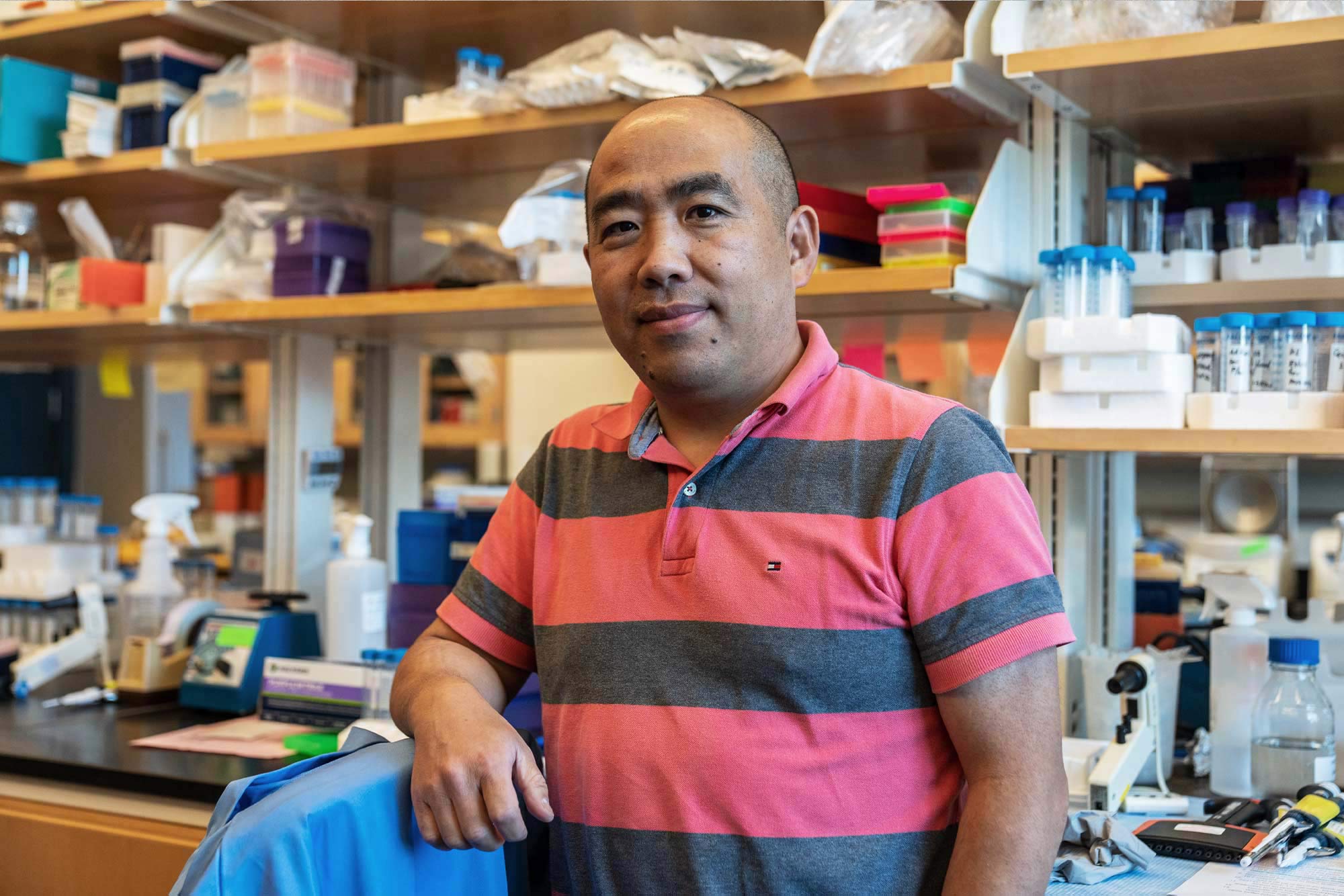
UVA researcher Jie Sun led the team that found that COVID-19 infection can cause sweeping changes in immune cells inside the lung tissues, promoting scarring and driving ongoing inflammation even after the initial infection has passed. This ongoing inflammation, they believe, drives the lasting respiratory symptoms, such as cough and difficulty breathing, associated with long COVID.
The new research from Sun and his colleagues indicates doctors may be able to halt the chronic inflammation using a class of drugs now used to treat rheumatoid arthritis, including baricitinib. The anti-inflammatory drugs previously received emergency authorization from the federal Food and Drug Administration to treat uncontrolled inflammation seen in severe COVID-19 infections.