A combination of inexpensive oral medications may be able to treat fatigue-inducing anemias caused by chronic diseases and inflammation, a new discovery from the University of Virginia School of Medicine suggests.
This type of anemia is the second-most common kind, and it can be an added burden for organ-transplant recipients and people with autoimmune disorders, as well as patients battling cancer, kidney disease and other conditions. In addition to causing severe fatigue, the anemia can trigger headaches, dizziness, rapid heartbeat and sweating.
“Not only do these anemias cause unpleasant symptoms, but they also are associated with functional impairment and shorter lifespan,” said researcher Dr. Adam Goldfarb, chief of UVA Health’s Division of Experimental Pathology. “Drawbacks of current therapies include their expense, tendency to lose of effectiveness and risk for serious side effects. This new therapeutic approach has the potential to provide a low-cost, highly effective, safe alternative.
“A further benefit would be its easy applicability to resource-limited areas around the world.”
Understanding Anemia
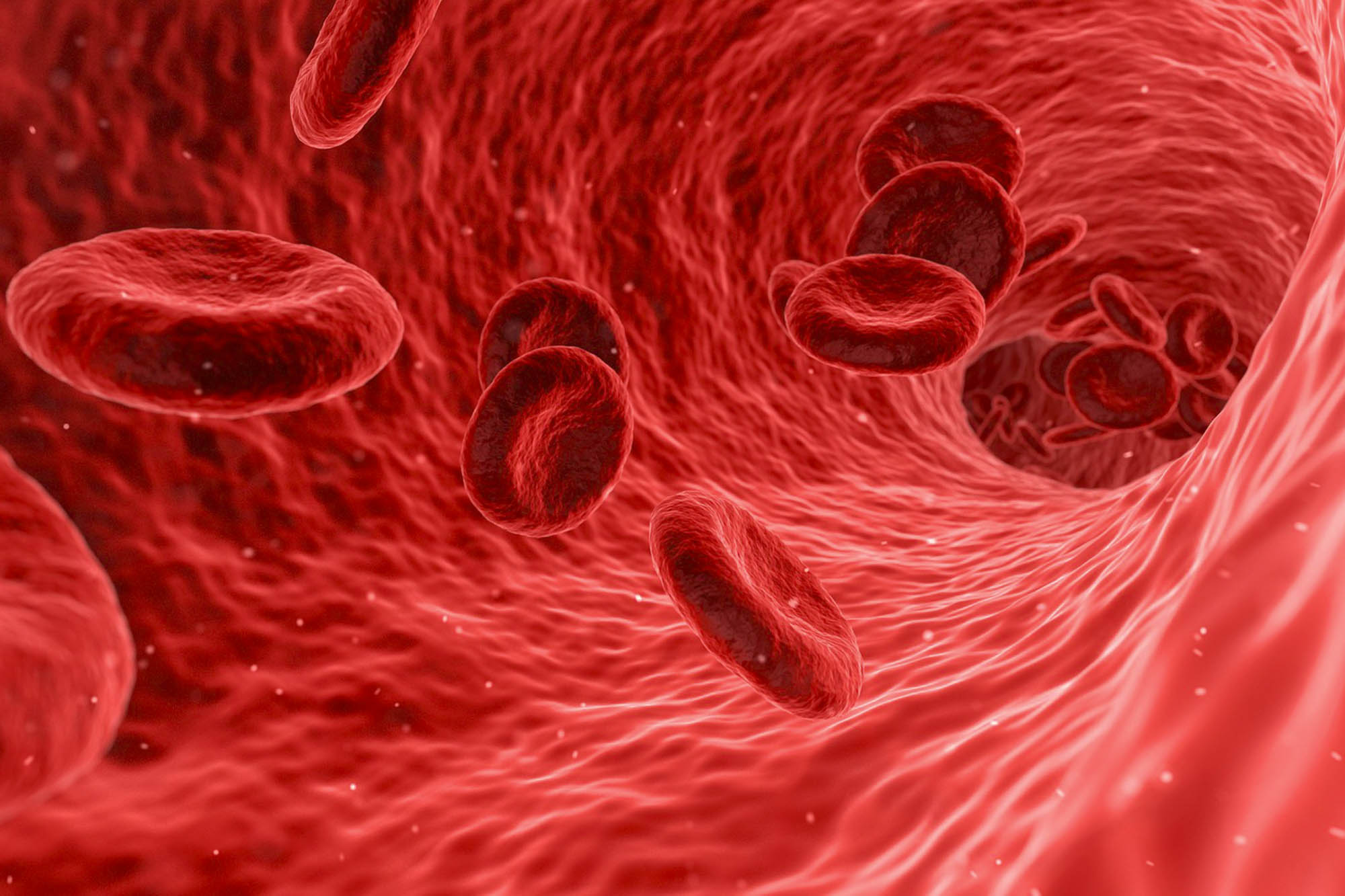
People with anemia have fewer red blood cells and less hemoglobin than normal. Red blood cells carry oxygen throughout the body, while hemoglobin is an iron-rich protein in the red blood cells that transports oxygen molecules.
There are several types of anemias, but anemia of chronic disease and inflammation is triggered by restricted iron delivery to the bone marrow cells that make red blood cells.
Goldfarb and his colleagues initially found that this inadequate availability of iron disrupts an important organelle inside our cells called the Golgi apparatus. This multi-layered organelle, which is shaped a bit like a ribbon candy, is responsible for packaging proteins and lipids (fats) vital to cells’ healthy operations.

Dr. Adam Goldfarb is chief of UVA Health’s Division of Experimental Pathology. (Contributed photo)
Their further studies identified the underlying source of this problem as a breakdown of tiny microtubules, which provide critical scaffolding for Golgi assembly and for the intracellular transport machinery. Importantly, the researchers were able to pinpoint the trigger for this microtubule breakdown as the loss of a protein, ferritin, within the cell.
By knowing the root cause of these cellular defects, the scientists could tailor a targeted approach to reverse the problem in mouse models of anemia. Giving the lab mice a combination of two substances, isocitrate and fumarate, allowed ferritin recovery and microtubule regrowth, enabling long-term correction of anemia caused by inflammation.
This suggests that an inexpensive oral medication might one day help human patients, too. Pilot studies in patients with anemia associated with kidney disease are in the advanced planning phase.
“The need for new anemia therapies is highlighted by the abundance of new agents currently in early clinical trials,” Goldfarb, of UVA’s Department of Pathology, said. “In defining a novel basic cellular response, our work has opened the door to a safe and simple therapy with unique potential for global accessibility.”
Findings Published
The researchers have published their findings in the scientific journal Nature Communications. The research team consisted of Goldfarb, Katie C. Freeman, Ranjit K. Sahu, Kamaleldin E. Elagib, Maja Holy, Abhinav Arneja, Renata Polanowska-Grabowska, Alejandro A. Gru, Zollie White III, Shadi Khalil, Michael J. Kerins, Aikseng Ooi, Norbert Leitinger, Chance John Luckey and Lorrie L. Delehanty.
The work was supported by the National Institutes of Health’s National Institute of Diabetes and Digestive and Kidney Diseases grants R01 DK079924 and R01 DK101550; the National Heart, Lung and Blood Institute, grant R01 HL149667; National Cancer Institute, grant P30 CA44579; UVA’s Medical Scientist Training Program, grant 5T32GM007267-38; and an National Institute of Diabetes and Digestive and Kidney Diseases Research Supplement to Promote Diversity in Health-Related Research, 3R01DK079924-09A1S1.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog.
Media Contact
Article Information
April 26, 2021
/content/anemia-discovery-points-more-effective-treatment-approaches