UVA Health researchers have discovered a molecule in the brain responsible for orchestrating the immune system’s responses to Alzheimer’s disease and multiple sclerosis, potentially allowing doctors to supercharge the body’s ability to fight those and other devastating neurological diseases.
The molecule the researchers identified, called a kinase, is crucial to both removing plaque buildup associated with Alzheimer’s and preventing the debris buildup that causes multiple sclerosis, or MS, the researchers found. It does this, the researchers showed, by directing the activity of brain cleaners called microglia. These immune cells were once largely ignored by scientists, but have, in recent years, proved vital players in brain health.
UVA’s important new findings could one day let doctors augment the activity of microglia to treat or protect patients from Alzheimer’s, MS and other neurodegenerative diseases, the researchers report.
“Our work further shows that targeting this novel pathway provides a potent strategy to eliminate the toxic culprits that cause memory loss and impaired motor control in neurodegenerative disease,” said senior researcher John Lukens of the University of Virginia School of Medicine and its Center for Brain Immunology and Glia, as well as the Carter Immunology Center and the UVA Brain Institute.
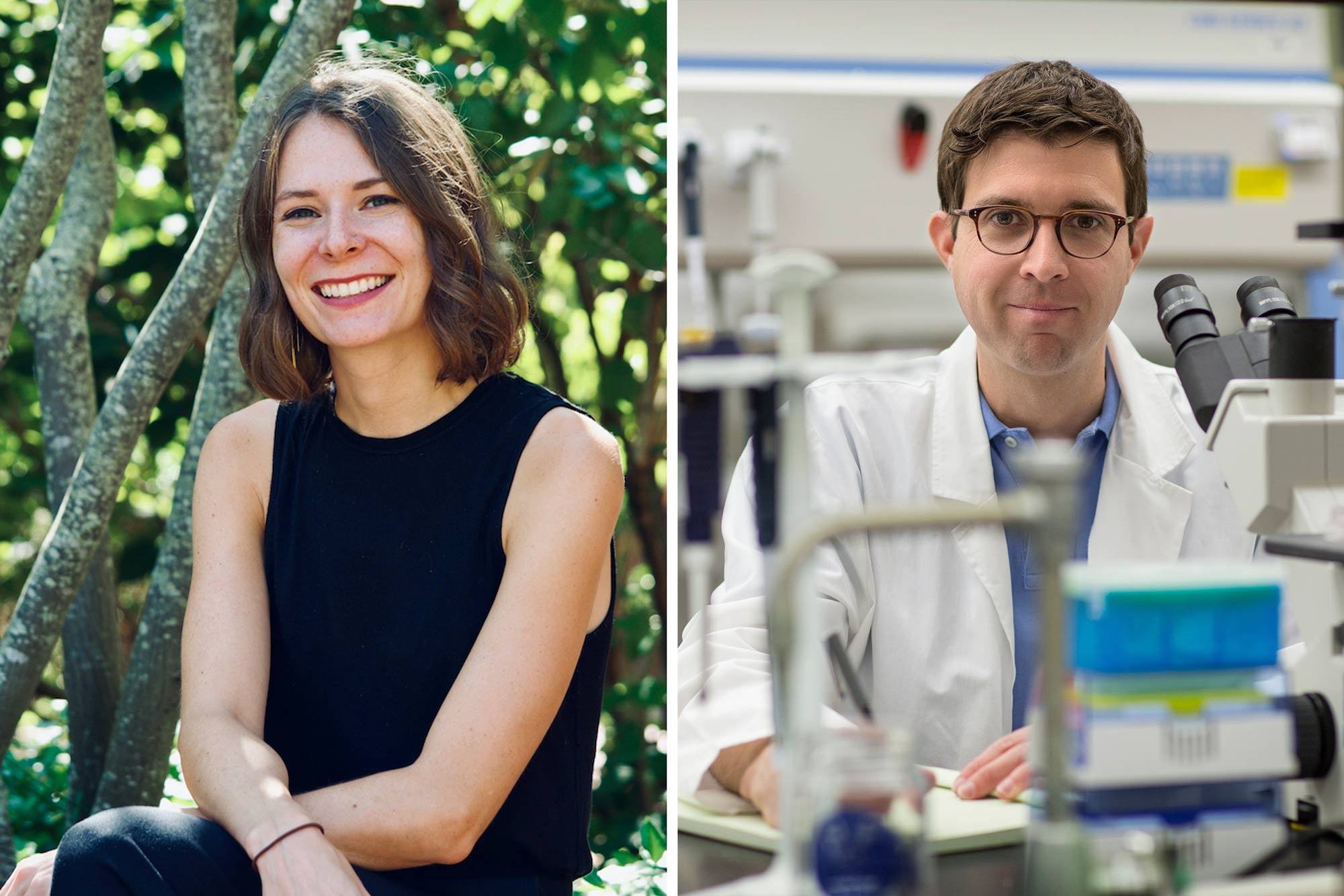
“In our studies, we have discovered a master controller of the cell type and processes that are required to protect the brain from these disorders,” Lukens said.
The discovery could also eventually protect patients from other disorders like Parkinson’s and amyotrophic lateral sclerosis, commonly called ALS or Lou Gehrig’s disease.
Toxic Brain Buildup
Many neurodegenerative diseases, including Alzheimer’s and MS, are thought to be caused by the brain’s inability to cleanse itself of toxic buildup. Recent advances in neuroscience research have shed light on the importance of microglia in removing harmful debris from the brain, but UVA’s new discovery offers practical insights into how this cleaning process occurs – and the dire consequences when it doesn’t.
Using a mouse model of Alzheimer’s disease, the UVA researchers found that a lack of the molecule they identified, spleen tyrosine kinase, triggered plaque buildup in the brain and caused the mice to suffer memory loss – like the symptoms seen in humans with Alzheimer’s. Further, the neuroscientists were able to reduce the plaque buildup by activating this molecule and microglia in the brain, suggesting a potential treatment approach for human patients, though that would require significantly more research and testing.
“Our work has described a critical element of microglial function during Alzheimer’s disease and MS,” said researcher Hannah Ennerfelt, the first author of a new scientific paper outlining the findings. “Understanding the underlying biology of these cells during neurodegeneration may allow for scientists and doctors to develop increasingly informed and effective therapeutic interventions.”
A lack of the molecule in a mouse model of MS, meanwhile, led to the buildup of damaged myelin, a protective coating on nerve cells. When myelin is damaged, the cells cannot transmit messages properly, causing MS symptoms such as mobility problems and muscle spasms. The UVA researchers conclude in a new scientific paper that the molecule they identified, abbreviated as SYK, is “critically involved” in the crucial removal of myelin debris.
“If boosting SYK activity in microglia can decrease the amount of myelin debris in MS lesions, developing new drugs to target SYK could stop the progression of MS and help to reverse the damage,” Elizabeth L. Frost, a researcher on the project, said. “This is an especially promising option given that most of the currently available drugs for MS treatment dampen adaptive immunity. These immunosuppressive drugs lead to susceptibility to infection and higher risk of potentially fatal side effects like progressive multifocal leukoencephalopathy. Additionally, some forms of MS do not have a strong involvement of the immune system, and therefore there are currently very limited treatment options for those patients.
“Targeting SYK in microglia,” she noted, “would circumvent multiple limitations of present-day therapeutics for MS.”
Based on their promising results, the researchers report that targeting the molecule to stimulate the brain’s immune activity could offer a way to treat not just Alzheimer’s and MS, but a “spectrum” of neurodegenerative diseases.
“These findings are especially exciting because they point to a treatment avenue in which we could alter the behavior of these native brain cells, microglia, to behave in a more neuroprotective way,” researcher Coco Holliday, a UVA undergraduate working in the Lukens lab, said. “It could potentially be applied to a variety of different neurological diseases that all share the problem of a buildup of toxic waste in the brain.
“It’s been a very exciting project to be a part of.”
Findings Published
The researchers have published their findings in the scientific journal Cell. The team consisted of Ennerfelt, Frost, Daniel A. Shapiro, Holliday, Kristine E. Zengeler, Gabrielle Voithofer, Ashley C. Bolte, Catherine R. Lammert, Joshua A. Kulas, Tyler K. Ulland and Lukens. The researchers reported no financial interests in the work.
The research was supported by the National Institutes of Health’s National Institute of Aging, grant RF1AG071996-01; the National Institute of Neurological Disorders and Stroke, grant R01NS106383; the Alzheimer’s Association, grant ADSF-21-816651; the Cure Alzheimer’s Fund; The Owens Family Foundation; and several training grants.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog.
Media Contact
Article Information
July 2, 2025