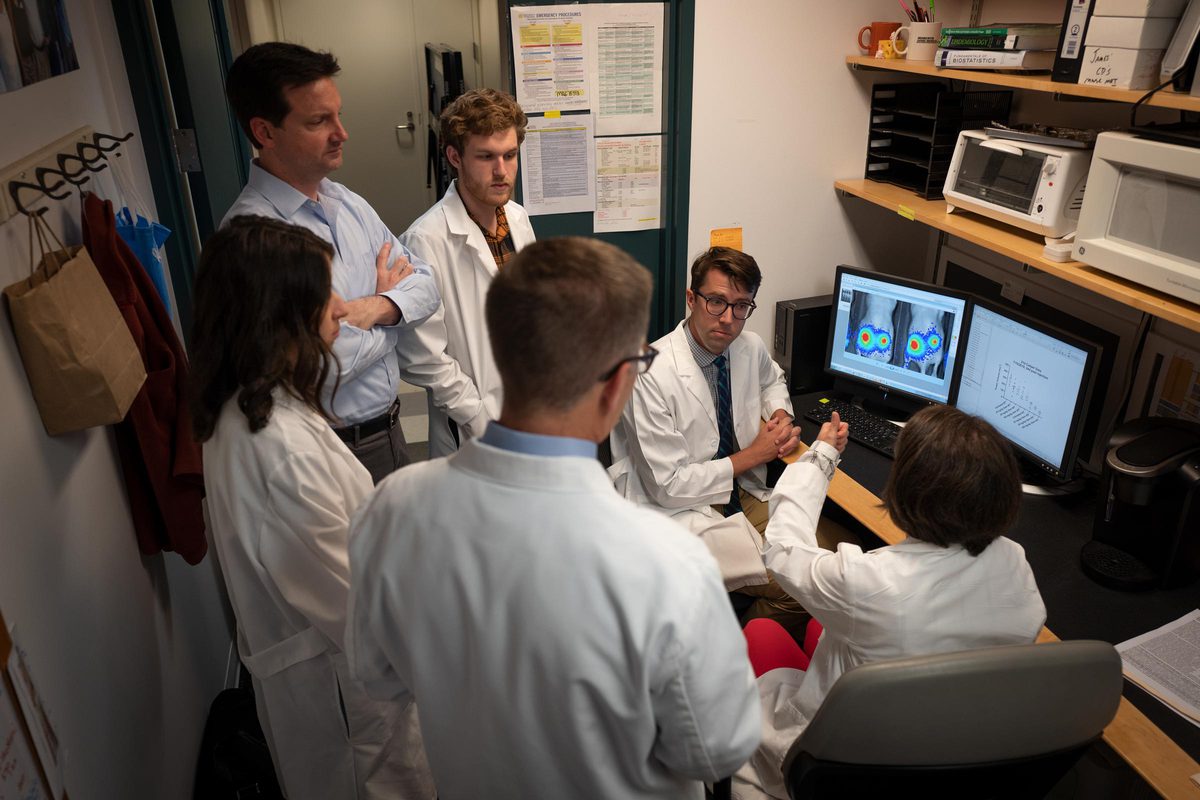
Lazzara and his team are studying the cell-signaling pathways that transmit information to cancer cells from many different sources simultaneously. These signals may influence a cell to divide, migrate, die or resist therapy.
“There are quantitative rules about that process, and we’re trying to decipher what those rules are,” Lazzara said. “We are on the threshold of quantitatively understanding how signaling pathways actually dictate what a cell will do in one context or another.
“What happens often in cancer is that a gene is mutated or over-expressed in a way that changes the way those signals are generated. And that then changes what a cell decides to do. It proliferates out of control or migrates when it’s not supposed to, and often becomes extremely resistant to chemotherapy.”
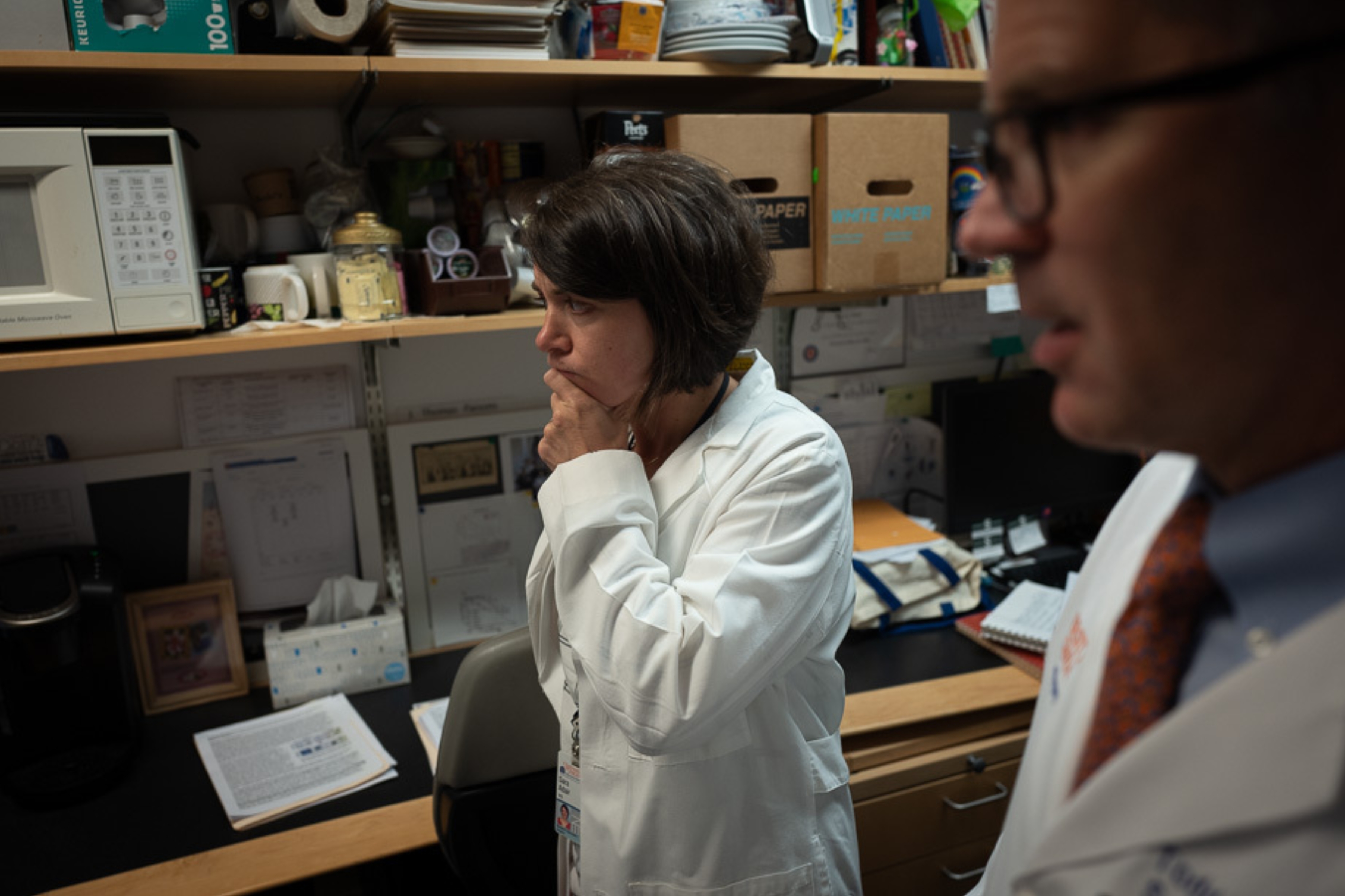
Stanger, co-investigator on the project, said cancers can outsmart drug regimens given to patients to fight the disease. “The goal of the grant is to understand the signals that underlie ‘plasticity,’ the capacity of cancer cells to change their properties to evade the anti-tumor effects of chemotherapy.”
At the University of Delaware, Ogunnaike develops and analyzes engineering control systems.
“There are certain drugs that have an effect on pancreatic cancer. Which ones to use, how much of each and when to apply them to the patient can be formulated in the form of an optimal control problem and solved using mathematical models,” Ogunnaike said. “My role in this project is to develop the mathematical models and apply principles of optimal control theory to determine the amount and timing of the therapeutics that Matt has identified as potential treatments.”
The research team is compiling tremendous amounts of data around what influences cell signaling and decision-making in pancreatic cancer. They feed that data into a model and use machine learning to look for unique patterns that might explain what they see happening. They are specifically looking at cells that decide to undergo a process called epithelial-mesenchymal transition, in which cells become migratory and invasive. In pancreatic cancer, these cells also become more resistant to chemotherapy.
“We think we’ve identified some of the pathways that regulate this transition to a more chemo-resistant state, and we think it may be possible to drug the cells back to an epithelial state, which will make them more sensitive to chemotherapy,” Lazzara said. “The extra piece of this grant, which I think made it attractive to the National Institutes of Health, is that after identifying which combination of drugs to use, we’re going to use a different kind of computational modeling to figure out how best to combine those drugs to minimize toxicity for patients.”
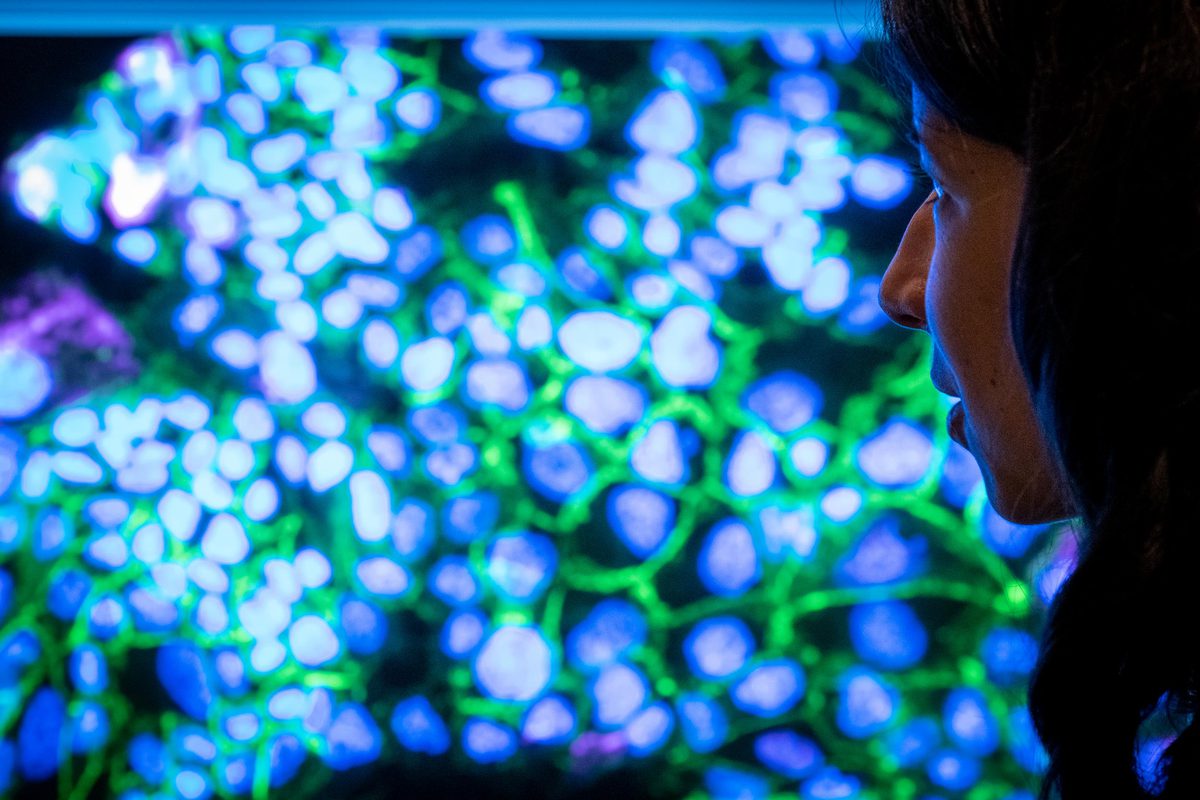
His team of researchers are hard at work. In Lazzara’s lab, Ph.D. student and National Science Foundation Graduate Research Fellow Brooke McGirr is analyzing pancreatic cells in sections of tumors grown in mice. Her research focuses on the cell-signaling processes regulated by the complex tumor microenvironment that drive epithelial-mesenchymal transition.
“I’m fascinated by the development of novel therapeutic regimens to give people hope and a better life,” she said. “I was drawn to work with Professor Lazzara because he works at the intersection of quantitative problem-solving and complex challenges in cancer biology.”