COVID-19 is surging in the United States and in Europe. The U.S. recorded 64,000 new cases and 517 deaths on Monday, continuing a generally upward trend since late summer. And 18 states recorded more infections last week than during any other seven-day period since the pandemic began. More than 8.3 million Americans are now known to have been infected.
Cases in Europe are rising even faster, as are hospitalizations, with Europe now surpassing the U.S. in COVID-19 cases per million population, leading countries to place new restrictions on business activities.
There are several reasons for the rapid increase in cases, including increased testing, but much of the surge may be the result of “pandemic fatigue” – people letting their guards down and getting back to business after months of restrictions intended to reduce infection rates.
The good news is that death rates are decreasing as clinicians improve treatments, and vaccines should soon become available.
Dr. William Petri, the Wade Hampton Frost Professor of Medicine at the University of Virginia and vice chair for research in the Department of Medicine, is studying the effects of COVID-19 on the immune system and seeking new treatments and vaccines.
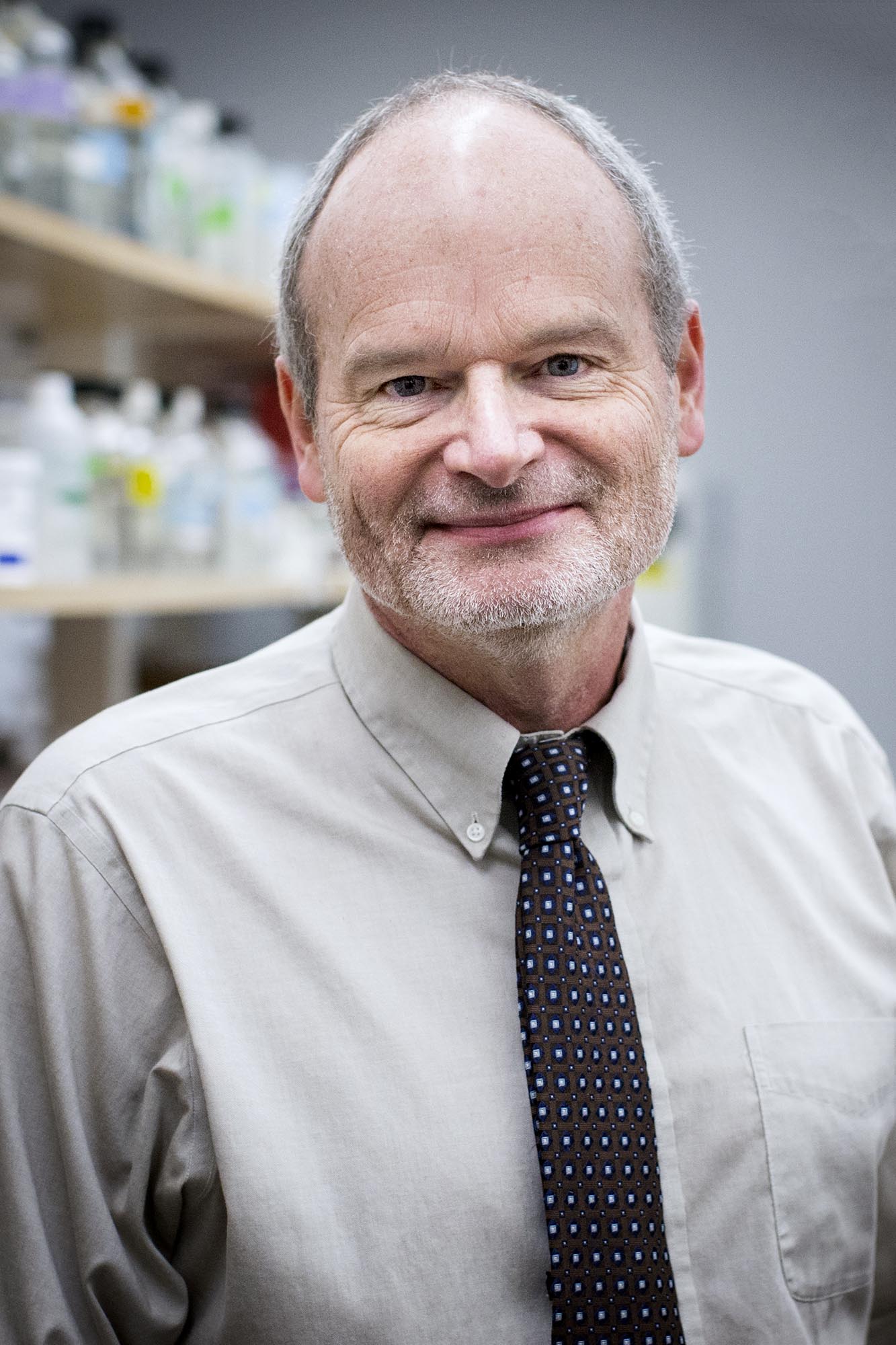
Dr. William Petri is studying COVID-19 and both new treatments and possible vaccines. (Photo by Sanjay Suchak, University Communications)
Here, he discusses the rise in COVID-19 cases.
Q. What are the reasons for the new global surge in COVID-19 cases?
A. The global surge is likely due to a combination of reopening the economies of nations; lack of universal adherence to prevention strategies that include face masks, social distancing and hand washing; outbreaks in nursing homes, prisons and colleges; the onset of colder weather in the Northern Hemisphere that leads to more indoor activities; lack of a vaccine; and inadequate case identification and contact tracing.
Q. Are you expecting a dramatic increase in hospitalized patients in the U.S.?
A. There has not yet been an increase in hospitalized patients, staying at about 200 per 100,000 of the population in the last two months. However, it unfortunately makes sense that hospitalizations will increase if the current trend toward increasing cases continues. Cases overall in the U.S. have nearly doubled since mid-summer. Perhaps mitigating this is the fact that the majority of infections are in people under 50 years old, an age group where disease is less severe.
Q. What can be done in the U.S. and elsewhere to tamp this down before it becomes a greater crisis?
A. Adherence to prevention strategies is key. These include isolating yourself at home if you have any symptoms that could be COVID-19 – these symptoms can include fever, cough, shortness of breath, loss of taste or smell, runny nose or congestion, nausea vomiting or diarrhea – and quarantining for two weeks if you have been in close contact with someone who has COVID-19. All of us should be using face masks, practicing social distancing and hand washing, sanitizing chairs and tables used in public, and interacting only in small groups of five to 10 people. Members of the University community should remember to complete the HOOS Health Check phone app each day.

It is difficult to prevent getting COVID-19 if you are caring for a family member or friend in your home; about one in five home caregivers become infected, despite all the above precautions.
I am leading the UVA part of a multi-center phase 3 study of a cocktail of anti-spike glycoprotein monoclonal antibodies for the prevention of household transmission of COVID-19. If this is shown to be successful, and if the cocktail can be mass-produced in adequate amounts, it would offer an additional approach to prevention before a vaccine becomes available.
Q. As treatments for COVID-19 improve and become more available, can we reduce hospitalizations and death rates even as the case counts rise?
A. Treatment of patients severe enough to be hospitalized has improved dramatically with the use of the anti-viral drug remdesivir and the anti-inflammatory drug dexamethasone. Dr. Patrick Jackson, an infectious diseases physician, led the UVA part of the phase 3 study of remdesivir, showing that the drug decreases length of hospital stay. A study in the United Kingdom has shown that dexamethasone decreases deaths in severe COVID-19 by a third. So treatment of the most severely ill has measurably improved with the advent of dexamethasone and remdesivir.
The COVID cocktail study team includes Bridgette Arlook, Christy Breeden, Rebecca Wade, Crystal Reed, Jennifer Pinnata, William Petri Jr. and Andrea Stanley. (Contributed photo)
Right now, we do not have FDA-approved therapies for outpatients to help limit the illness and keep them from being hospitalized; however the Regeneron cocktail of anti-spike glycoprotein monoclonal antibodies that I am studying – should it get emergency use authorization from the FDA – would be the first such drug, as it has been shown to decrease viral load and days of symptoms.
The antibody cocktail could be widely available and easily used, as we have lots of experience in using antibodies to treat other diseases such as rheumatoid arthritis and atopic dermatitis, so this experience will facilitate the use of the cocktail.
What will limit the use is production – right now, the U.S. government has purchased 50,000 doses and has plans for hundreds of thousands of doses. But before there is a vaccine, the demand for the antibody cocktail could exceed millions of doses. However, other companies, including Eli Lilly, also have anti-spike antibody treatments in clinical trials which will likely help, too.
Q. What will it take to bring this pandemic to an end?
A. A combination of vaccination, case identification and contact tracing, and maintaining mask wearing, social distancing and diligent hand washing.
The pandemic will be a memory in a year, I believe, as by the end of next summer we will have widespread vaccination. However, it seems likely that COVID-19, while no longer a pandemic, will be part of cold and flu season each year, requiring us to maintain vaccination and vigilance.
Media Contact
Article Information
October 20, 2020
/content/qa-dr-william-petri-coming-covid-19-surge

