You might think a Pfizer vice president overseeing key processes in the production of his company’s COVID-19 vaccine would know how clinical studies were going, but access to such information could violate insider-trading laws.
So Paul Mensah, a University of Virginia chemical engineering alumnus, learned like most Americans the morning of Nov. 9 how the thing that consumed his days and nights for eight months was really going to work.
“I heard it on the news,” Mensah recalled of the day Pfizer announced the vaccine proved more than 90% effective in Phase 3 trials. “And when I came to my computer, there was an email from our CEO and our head of research sharing the excitement about the data.”
Then, his wife and children were there hugging him – and not just in congratulations. They were thanking him, too, for his efforts to make a vaccine available. It was a feeling Mensah did not take for granted, in spite of 5 a.m. conference calls and 17-hour days glued to his computer.
Mensah, who earned his Master of Science and Ph.D. at UVA in 1997 and 1999, respectively, oversees Pfizer’s bioprocess research and development and drug supply group. The group is responsible for the development and manufacturing of drug substances, which are the active ingredients in pharmaceutical products. In Pfizer’s COVID-19 formulation, that ingredient is the messenger RNA upon which the vaccine is based.
“I can speak for my group, and perhaps everyone at Pfizer, that working on the vaccine is personal, and in many ways, a privilege as well,” Mensah said. “It’s personal because all of humanity needs the vaccine. But it’s also a once-in-a-lifetime opportunity where you can look back and say you helped with this pandemic, and the efforts were successful. It’s been hugely inspirational and hugely motivational.”
Mensah is among a group of UVA Engineering faculty, alumni and students who have important roles in the fight against COVID-19. They are attacking the pandemic from all angles – investigating antiviral drugs, tracking data and protecting supply chains of vaccines, tests and treatments from those who would do harm.
Michael L. King, who received his Master of Science in chemical engineering at UVA in 1976, is a professor of practice in the department and a retired Merck and Co. vice president. He also is a subject matter expert in vaccine development and distribution for the Bill & Melinda Gates Foundation, a leader in global efforts to end the pandemic.
Like Mensah, King understands the reality that vaccinating about 80% of the world’s nearly 8 billion people is the only way to stop COVID-19. So do chemical engineering alumnus Drew Biedermann and student Nick Seyler.
Biedermann earned his B.S in chemical engineering at UVA in 2017 and now works in the chemical engineering lab of professor Chris Love at Massachusetts Institute of Technology; Love also happens to be a UVA alumnus with a bachelor’s in chemistry. Seyler is a fourth-year chemical engineering and biology undergraduate.
What unites these individuals – apart from ties to UVA’s Department of Chemical Engineering – is they’re all runners in the race to inoculate the world against COVID-19. Here are their stories.
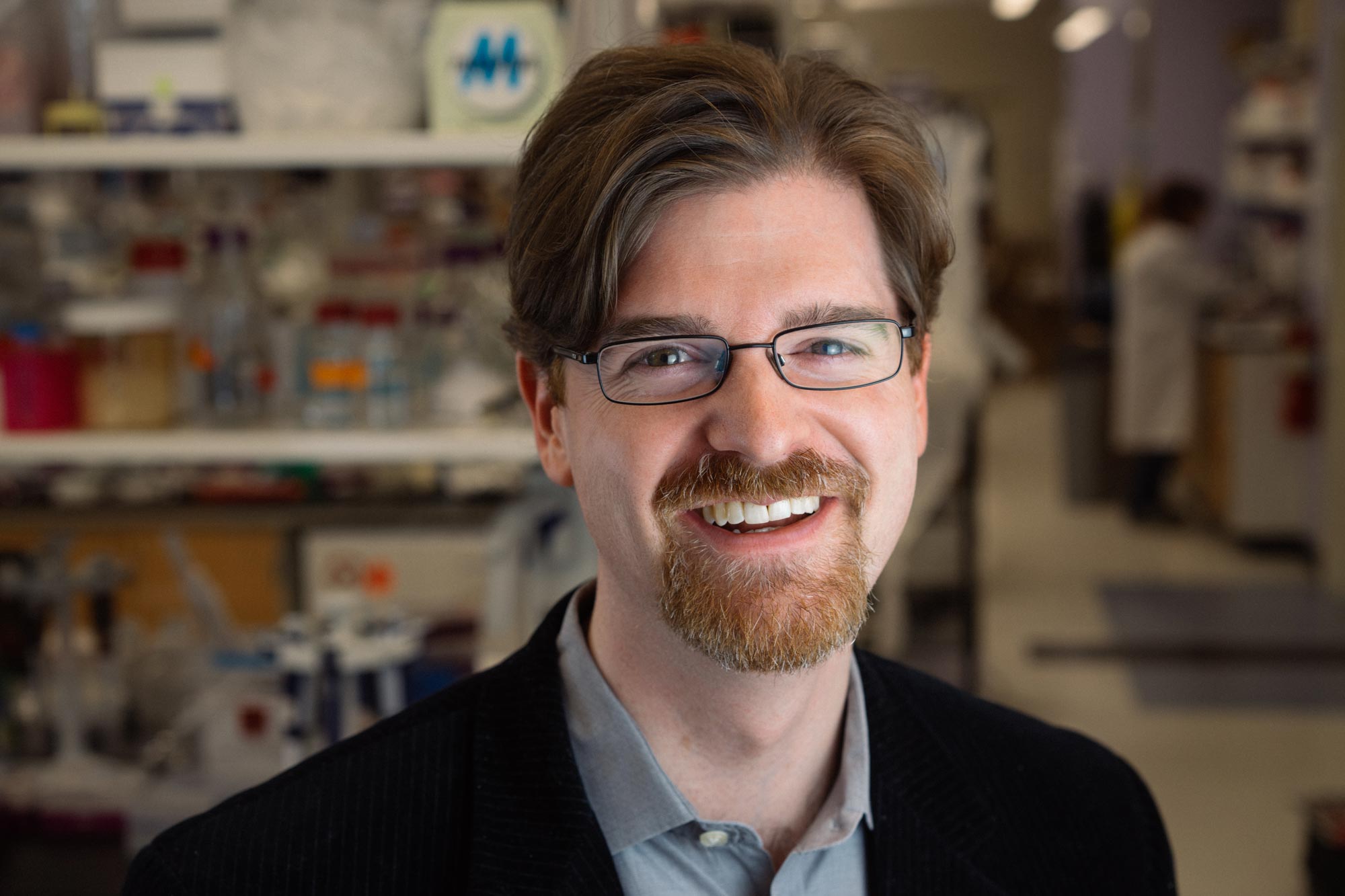
Michael L. King
On Feb. 21, 2020, King flew to Seattle to meet with colleagues from the Gates Foundation. King, who joined the UVA chemical engineering faculty in 2007 after 32 years at Merck, went to Seattle to discuss how he could help the foundation’s response to COVID-19, which still had not been declared a pandemic.
In April, the World Health Organization, the European Commission, France and the Gates Foundation launched the Access to COVID-19 Tools Accelerator, a collaboration of governments, businesses, scientists and non-governmental and global health organizations. The accelerator’s mandate is to speed up development, production and equitable access to COVID-19 tests, treatments and vaccines.

Michael L. King, professor of practice in UVA’s Department of Chemical Engineering, retired from Merck and Co. after 32 years in vaccine development and commercialization. (Contributed photo)
The vaccines pillar, called COVAX, is chartered under the World Health Organization, and two of its ACT Accelerator partners, the Coalition for Epidemic Preparedness Innovations and Gavi, The Vaccine Alliance. COVAX is an association of more than 185 member nations established to develop a portfolio of COVID-19 vaccines with the goal of ending the acute phase of the pandemic. COVAX, guided by the principle that no one is safe until everyone is safe, plans to distribute 2 billion doses to the most vulnerable people by the end of 2021.
King worked with the Gates Foundation and the Coalition for Epidemic Preparedness Innovations figuring out where to focus resources among hundreds of vaccine programs. He began by surveying 300 organizations worldwide to identify high-capacity manufacturers, and matching vaccine developers to antigen researchers in academia, such as Biedermann and Love. Ultimately, vaccinating enough people worldwide to contain COVID-19 will require many manufacturers and numerous technologies.
In mid-summer, King joined a multidisciplinary investment committee that manages allocations of funds under COVAX’s Research, Development and Manufacturing Workstream. He also serves on the committee’s Technical Review Group, which brings manufacturers, regulators and other stakeholders together to rapidly overcome common challenges.
“We workshop best practices for things like storage or labeling, so everybody’s not reinventing the wheel,” King said.
From his home office – where a Dr. Anthony Fauci bobblehead adorns the desk and photographs from his travels during easier times line the walls – King sits at a virtual table with people oceans away hashing out supply chains and regulatory approvals and manufacturing capacity. The hours can be long and stressful, but broken up by occasional levity, he said.
Once, King was leading a meeting of 40 or so people when a dog in New York wouldn’t stop barking. A dog on the West Coast started barking back. Far from being annoyed as the canines’ owners frantically tried to quiet them, someone said, “No, let’s hear what they have to say.”
“It just kind of broke the tension,” King recalled.
For King, seeing so many people work behind the scenes for the common good is heartening.
For example, to address glass vial shortages, developers agreed to retool for multi-dose packaging – cutting glass requirements by an order of magnitude, King said. Garnering that kind of cooperation isn’t automatic, though.
“To be effective, you have to understand other people’s perspectives, use your technical knowledge but also learn theirs well enough to find the sweet spot between the two,” he said, “and be an active listener. To get things done, leadership and teamwork are as important as technical skills.”
The pandemic response provided an excellent case study for students in King’s spring vaccines course, “Bioproduct and Bioprocess Engineering.” His role in COVAX gave students a unique perspective as events unfolded, so much so that he plans to revise the course content around COVID-19.
COVAX also reunited King with many colleagues from his time at Merck, whose expertise he relied on then, as he does now.
“It’s a small community, but we know and trust each other, and we work well together,” King said. “My students can see that maintaining professional networks is very important to be successful, so when things come up, they can always reach out to the right people.”
Andrew “Drew” Biedermann and J. Christopher Love
The Love Lab at MIT has worked with the Gates Foundation since 2017 to make extremely low-cost vaccines by investigating how to automate the first steps of manufacturing – finding materials in the lab likely to produce a strong immune response and modifying the materials to be ready for manufacturing. It was Valentine’s Day when the foundation called: Could Love and his students apply their ideas to a COVID-19 vaccine?
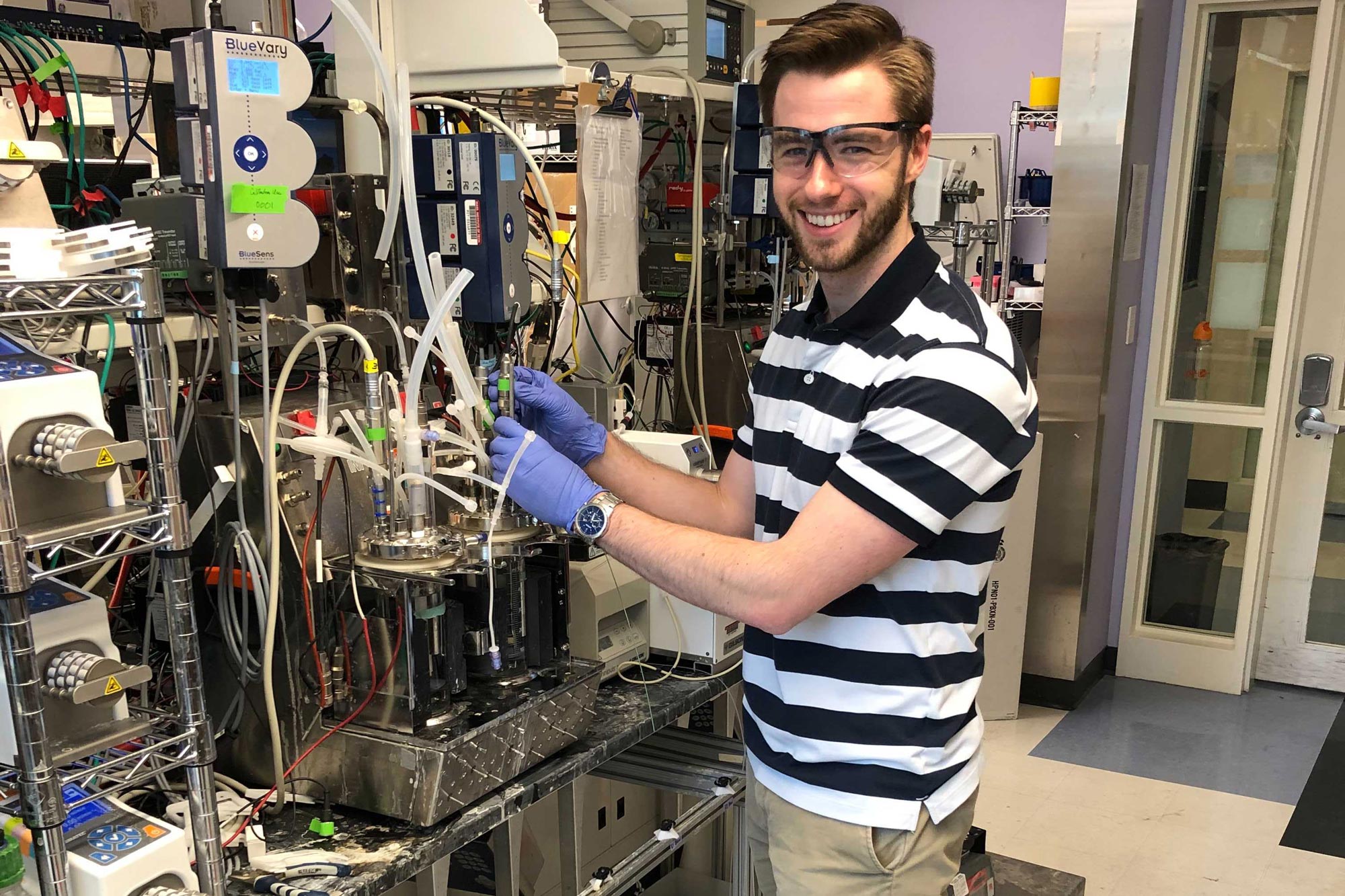
2017 graduate Andrew “Drew” Biedermann is a Ph.D. student in the chemical engineering lab of UVA alumn J. Christopher Love at MIT, developing low-cost subunit vaccine candidates and manufacturing methods. (Contributed photo)
“We’re developing more efficient ways of making vaccines, and one thing that goes hand-in-hand with that is speed,” said Biedermann, a former Rodman Scholar and a 2017 Outstanding Student Award winner, one of UVA Engineering’s highest undergraduate honors. “We think a lot about technologies that allow us to quickly develop new vaccine candidates.”
The team works on subunit vaccines, which use a piece of a protein from the virus – the antigen – to trigger the immune system to produce antibodies against the virus. One way they speed up the process is by using a fast-growing yeast host to produce a protein. The faster the protein-expressing yeast cells grow, the sooner the researchers can test the protein’s potential to spark an immune response, allowing them to move quickly through candidates.
One overarching goal is to build a system for on-demand drug development. The concept originated as a U.S. Department of Defense project a decade ago, and drew the attention of the Gates Foundation for its potential to produce vaccines for pennies per dose.