A UVA Health-developed drug delivery system using nanotechnology, designed to save patients from repeated surgeries, has shown surprisingly long-lasting benefits in lab tests – a promising sign for its potential to help human patients.
The approach allows surgeons to apply a paste of nanoparticles, tiny particles that are invisible to the human eye, on transplanted veins to prevent the formation of harmful blockages inside the veins. These blockages often force cardiac and dialysis patients to undergo multiple surgeries. Some dialysis patients need seemingly endless procedures on both arms, and then a leg or around their collarbone, so they can continue to receive lifesaving treatment.
While UVA’s innovation, dubbed “Pericelle,” has produced encouraging early results, there have been questions about how long the benefits could last. Not only did Pericelle work at three months – when the applied drug supply ran out – but it was still working at nine months.
“This is a big deal because the treatment could work much longer than we originally thought, far beyond what people would expect,” said researcher Lian-Wang Guo, who is developing the technique with UVA Health’s Dr. K. Craig Kent. “It is so exciting that one treatment can prevent the harmful blockages for many months.”
A $5 Billion Health Care Drain
Kent, a vascular surgeon and UVA Health’s chief executive officer as well as UVA’s executive vice president for health affairs, is well-acquainted with the challenges associated with “revascularization” procedures used to treat cardiovascular disease by restoring needed blood flow.
The procedure is also used to create access points for patients who need dialysis. An artery and vein in the arm, for example, are often grafted together so a patient’s blood can be removed from the body, cleansed and then returned. Management of these dialysis connection points, called arteriovenous fistulas, in patients with end-stage renal disease is estimated to cost the U.S. health care system $5 billion every year.
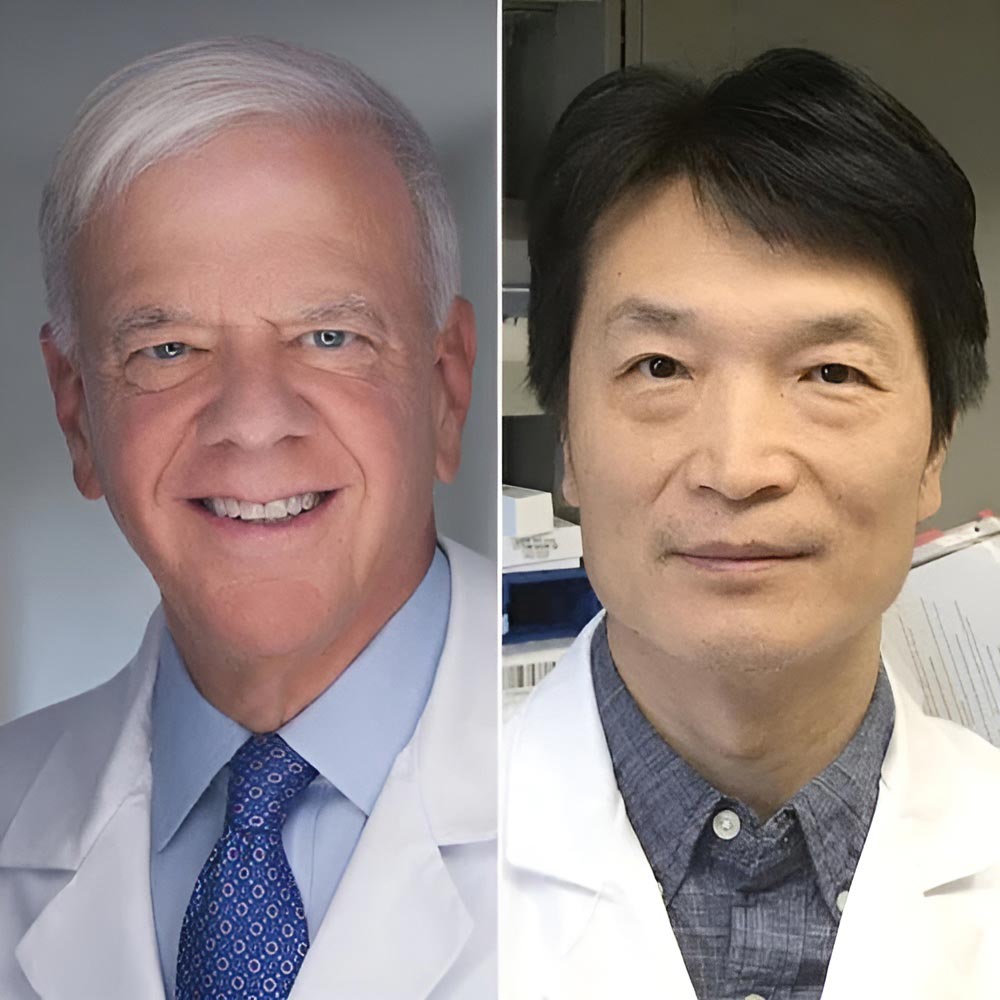
UVA Health’s Dr. K. Craig Kent, left, is a vascular surgeon, UVA Health’s CEO and UVA’s executive vice president for health affairs. He is working with UVA Health researcher Lian-Wang Guo, who is developing the technique. (Contributed photos)
Revascularizations can cause the very problem they’re trying to fix: inadequate blood flow. The surgery itself causes a buildup of cells in the blood vessels, choking off the blood supply.
“Repeated surgeries for vascular access and revascularization are not just a major burden for patients, they represent an urgent, unmet need in medicine,” Kent said. “The strain on patients’ lives and the health care system is immense, and innovative solutions like Pericelle offer an opportunity to change this paradigm. We desperately need alternatives that can deliver durable, long-term results.”
Kent, Guo and collaborator Shaoqin Gong, a University of Wisconsin-Madison researcher, hope Pericelle will be the answer. Surgeons would apply the hydrogel paste on blood vessels to deliver a drug, rapamycin, that can prevent the growth of invasive cells.