University of Virginia School of Medicine researchers have discovered a gene on the Y chromosome that contributes to the greater incidence of heart failure in men – and a possible treatment method.
Kenneth Walsh and his team have discovered how Y chromosome loss triggers changes in heart immune cells that make the cells more likely to cause scarring, which can lead to heart failure.
The researchers also found they could reverse the harmful heart changes by giving lab mice a drug that targets the process of fibrosis that leads to the heart scarring, which could lead to a similar treatment for men.
Y chromosome loss in men occurs progressively throughout life and can be detected in approximately 40% of 70-year-old men. Walsh discovered in 2022 that this loss can contribute to heart muscle scarring and lead to deadly heart failure.
That finding was the first to directly link Y chromosome loss to a specific harm to men’s health; Y chromosome loss is increasingly thought to play a role in diseases ranging from Alzheimer’s to cancer.
“Our previous work identified that it was loss of the entire Y chromosome that contributed to heart disease in men,” Walsh, the director of UVA’s Hematovascular Biology Center, said. “This new work identified a single gene on the Y chromosome that can account for the disease-promoting effects of Y chromosome loss.”
About Y Chromosome Loss
Unlike women, who have two X chromosomes, men have an X and a Y. For a long time, the genes found on the Y chromosome were not thought to play important roles in disease. Sex hormones, scientists thought, explained the differences in certain diseases in men and women.
But Walsh’s groundbreaking work has helped change that perception. It also suggested an explanation for why heart failure is more common in men than women. Cardiovascular disease, which includes heart failure, is the leading cause of death worldwide.
Y chromosome loss occurs in only a small percentage of affected men’s cells. This results in what is called “mosaicism,” where genetically different cells occur within one individual. Researchers aren’t entirely sure why this partial Y chromosome loss occurs, but predominantly it strikes elderly men and men who smoke compared to those who don’t.
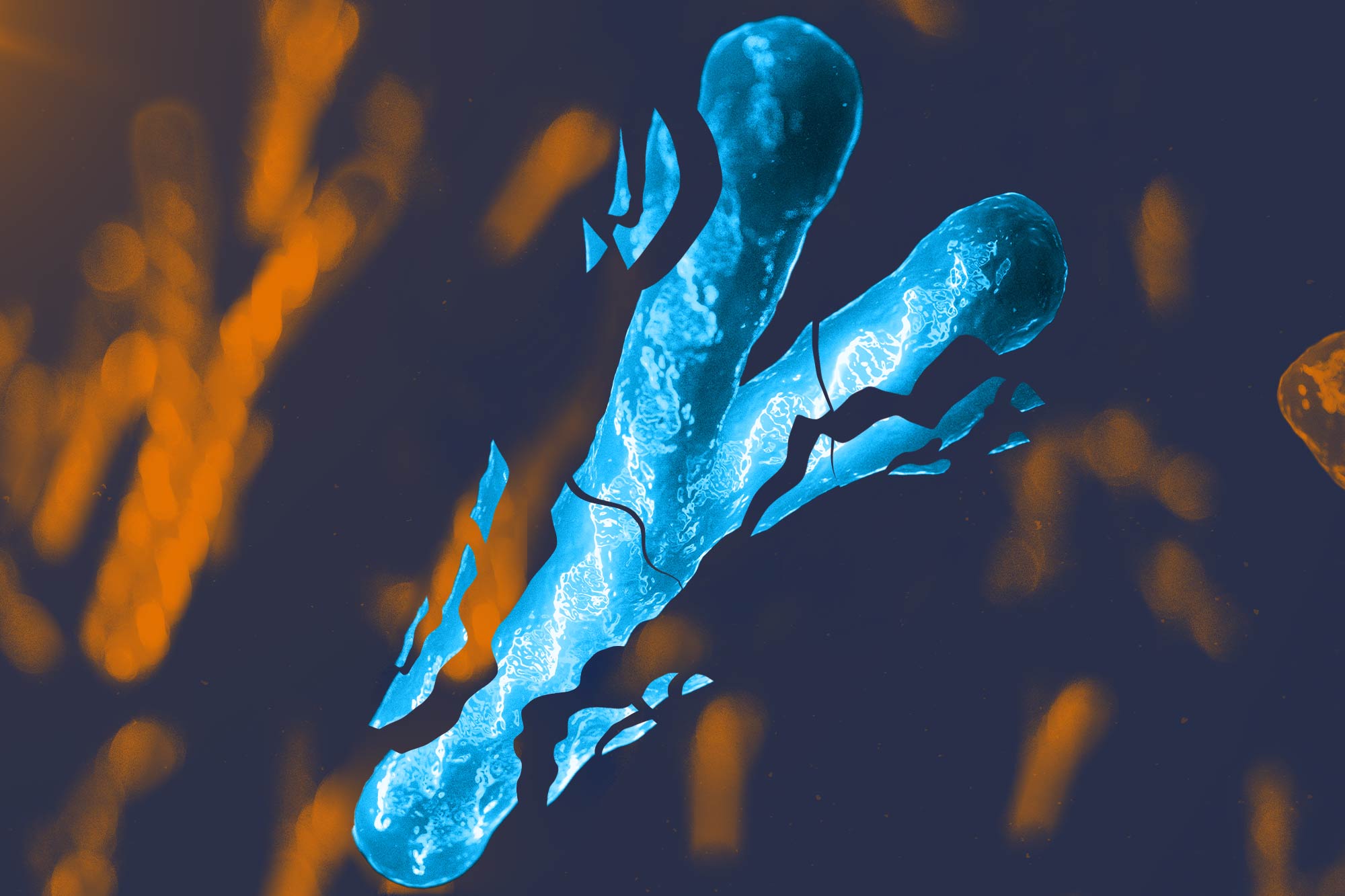
To better understand the effects of Y chromosome loss, Walsh and his team examined genes found on the Y chromosome to determine which might be important to heart scarring. One gene they looked at – “Uty” – helps control the operating instructions for immune cells called macrophages and monocytes, the scientists determined.
When the gene was disrupted, either individually or through Y chromosome loss, that triggered changes in the immune cells in lab mice. Suddenly, the macrophages were much more “pro-fibrotic,” or prone to scarring. This accelerated heart failure as well, the scientists found.

Researcher Kenneth Walsh says the discovery builds off of his team’s previous work that identified the loss of the entire Y chromosome as contributing to heart disease in men. (Photo by Dan Addison, University Communications)
“The identification of a single gene on the Y chromosome provides information about a new druggable target to treat fibrotic diseases,” said Walsh, who is also with UVA’s Division of Cardiovascular Medicine and Robert M. Berne Cardiovascular Research Center.
Walsh and his team were able to prevent the harmful changes in the mice’s macrophages by giving them a specially designed monoclonal antibody. This halted the harmful changes in the heart, suggesting the approach might, with further research, lead to a way to treat or avoid heart failure and other fibrotic diseases in men with Y chromosome loss.
“Currently, we are working with our clinician colleagues in the Division of Cardiovascular Medicine at UVA to assess whether loss of the Y chromosome in men is associated with greater scarring in the heart,” Walsh said. “This research will provide new avenues for understanding the causes of heart disease.”
Based on their findings, Walsh and his team believe that a small group of genes found on the Y chromosome may have big effects on a wide array of diseases. Their new work identifies mechanisms that may lead to this, and they are hopeful that further research will provide a much better understanding of unknown causes of sickness and death in men.
“This research further documents the utility of studying the genetics of mutations that are acquired after conception and accumulate throughout life,” Walsh said. “These mutations appear to be as important to health and lifespan as the mutations that are inherited from one’s parents. The study of these age-acquired mutations represents a new field of human genetics.”
Findings Published
The researchers have published their findings in the scientific journal Nature Cardiovascular Research. The team consisted of Keita Horitani, Nicholas W. Chavkin, Yohei Arai, Ying Wang, Hayato Ogawa, Yoshimitsu Yura, Megan A. Evans, Jesse Cochran, Mark C. Thel, Ariel H. Polizio, Miho Sano, Emiri Miura-Yura, Yuka Arai, Heather Doviak, Arthur P. Arnold, Bradley D. Gelfand, Karen K. Hirschi, Soichi Sano and Walsh. The scientists have no financial interest in the work.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog.