Pioneering researchers at the University of Virginia Cancer Center are developing innovative ways to supercharge our natural immune systems to defeat cancer and save lives.
Cancer is an elusive disease – one that can hide from our body’s immune defenses and even hijack those defenses for its own purposes. It’s consistently one of the top causes of death for Americans, with more than a half-million people dying from it each year.
To battle the disease, doctors have long relied on the twin cudgels of chemotherapy, to poison the cancer cells; and radiation, to blast them to death. The treatments can be lifesaving, but they also carry terrible side effects.
UVA’s Dr. Daniel “Trey” Lee and Dr. Lawrence G. Lum and their colleagues are developing elegant alternatives that empower our immune systems to recognize and destroy cancer. Cancer “immunotherapy,” as it is called, works by weaponizing immune cells to perform what are, in essence, highly precise drone strikes on cancer cells.
“Our immunotherapy research program allows us to offer patients alternatives they can’t find at most other hospitals,” explained Dr. K. Craig Kent, chief executive officer of UVA Health and executive vice president for health affairs at UVA. “Dr. Lee and Dr. Lum are true leaders in their fields, and their efforts are set to improve care not just for patients here at UVA Cancer Center, but throughout Virginia.”
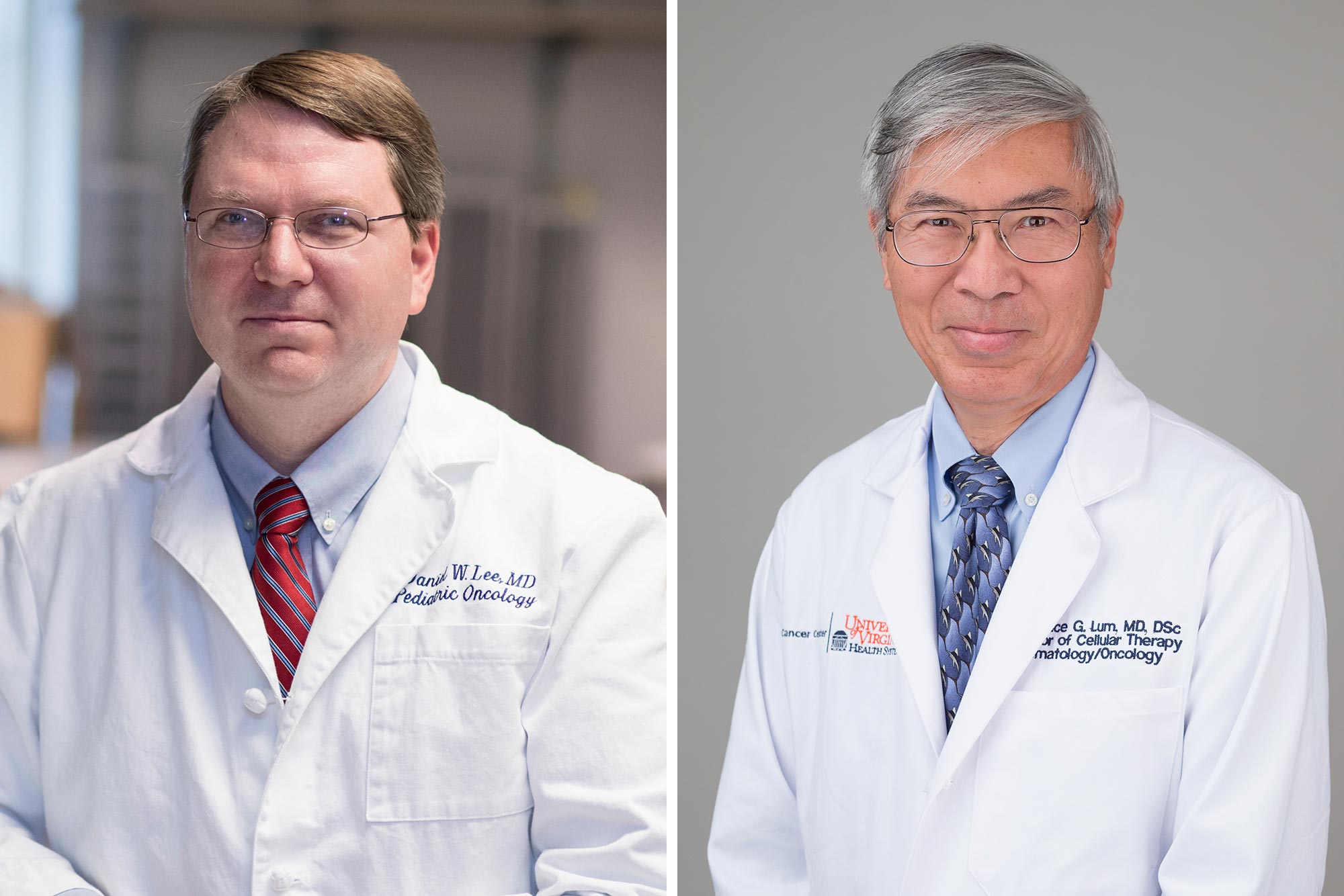
Dr. Daniel “Trey” Lee, left, and Dr. Lawrence G. Lum and colleagues are developing alternatives that empower our immune systems to recognize and destroy cancer. (Left photo by Dan Addison, University Communications; right photo courtesy UVA Health)
Lee’s approach, known as chimeric antigen receptor (CAR) T-cell therapy, involves extracting a small number of white blood cells called T cells from a patient’s blood, then genetically modifying them to kill cancer. Those cells are then infused back into the patient. The entire process takes about two weeks, as opposed to other processes that can take months.
The genetically engineered CAR T cells continue to replicate in the body, generating a population of hundreds of millions within a few days – a veritable army of cancer killers.
“No other therapy for cancer can expand inside the body once it is given,” said Lee, a pediatric oncologist at UVA Children’s and UVA Cancer Center. “That is the real power of CAR T-cell therapy – it replicates itself automatically until all the tumor is gone, then it kind of just goes away.
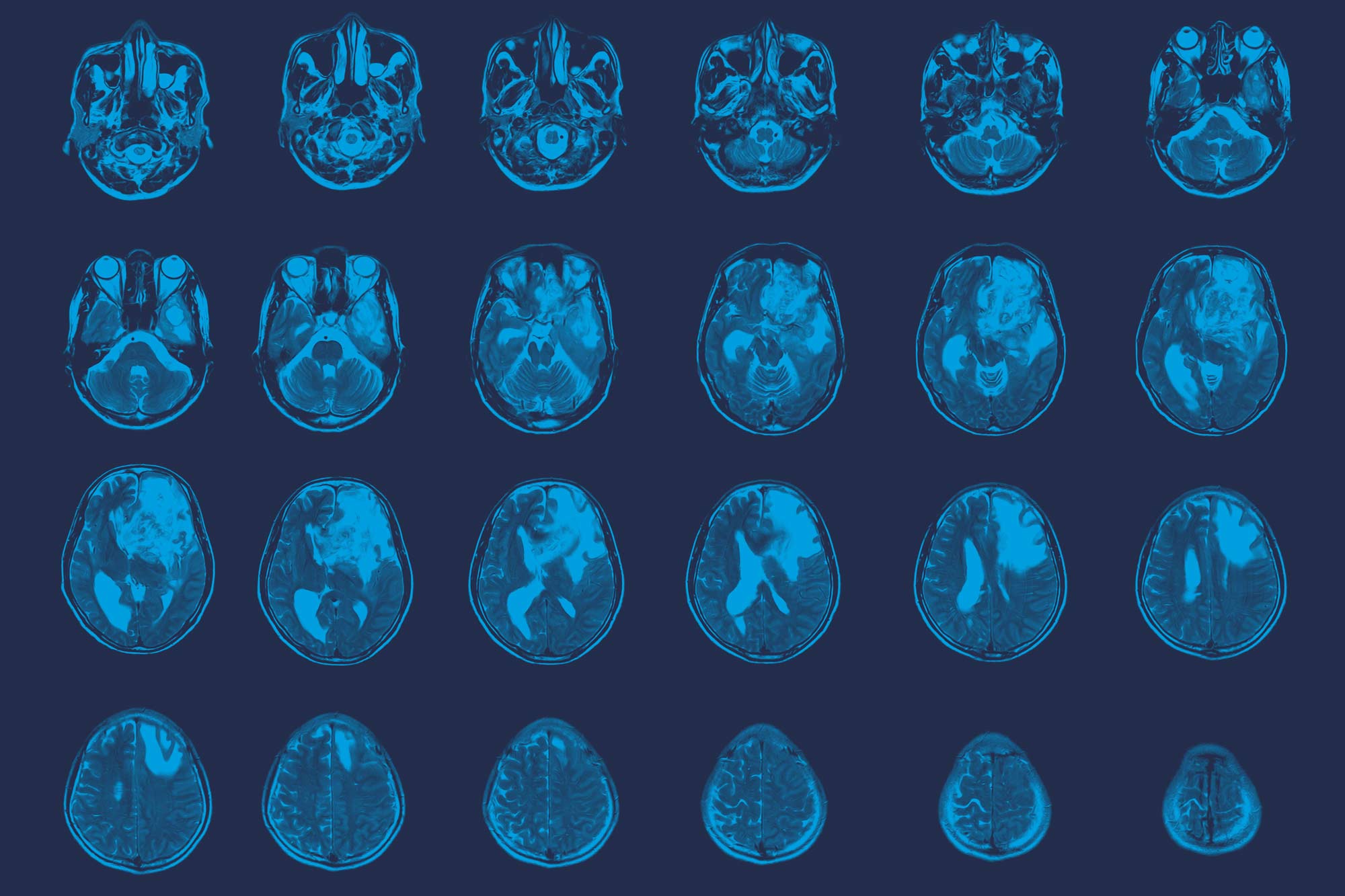
“CAR T-cell therapy has redefined the paradigm for how we treat children and adults with leukemia and lymphoma. So many children are alive today because of this. But patients with other tumors desperately need help, which is why my team at UVA is extending CAR T-cell therapy to the devastating brain tumors glioblastoma and DIPG.”