New digital twin technology that allows a University of Virginia-developed artificial pancreas system to adapt to users’ changing needs – and lets users adjust the settings – has been shown to improve Type 1 diabetes control, a study finds.
Called “adaptive biobehavioral control,” the technology helps fine-tune UVA’s artificial pancreas every two weeks, giving users a virtual tool to test different ways to manage their blood sugar using their own data. In a six-month study, participants using the technology spent more time in a healthy blood-sugar range, rising from 72% to 77%, and saw a small but meaningful drop in their average blood-sugar levels.
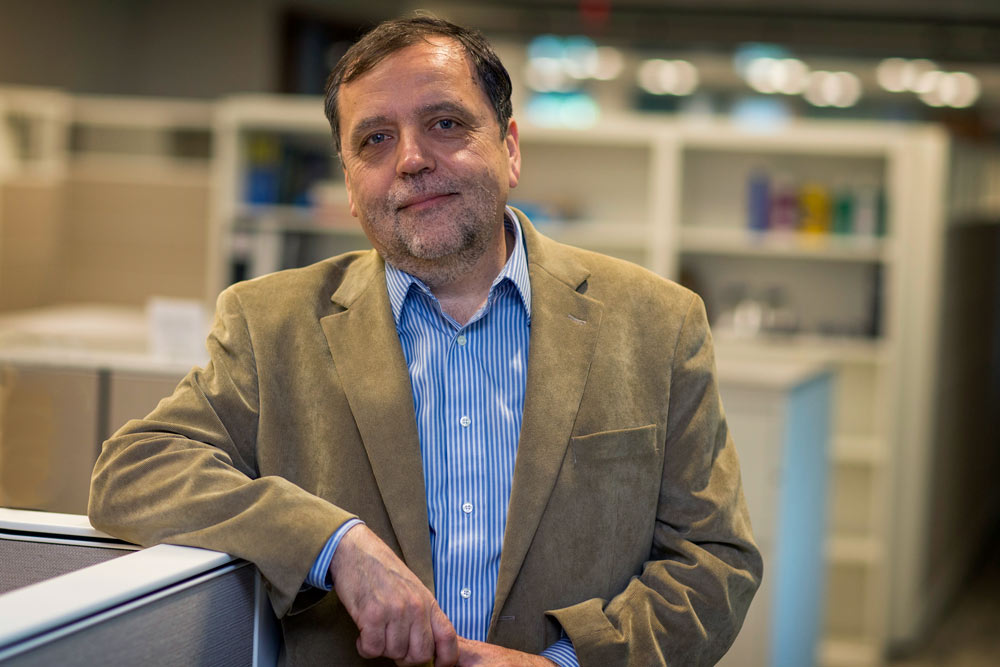
Boris Kovatchev, director of UVA’s Center for Diabetes Technology, says digital twin technology helps users and artificial pancreases adapt together for better diabetes control. (University Communications photo)
“Artificial pancreas systems require adjustments by those who use them to adapt to a person’s changing insulin demands,” said Boris Kovatchev, director of the UVA Center for Diabetes Technology. “This is the first study that maps each person to their ‘digital twin’ in the cloud and enables people with diabetes to experiment with their own data to learn how their artificial pancreas system would react to changes, in a safe simulation environment, before adjusting their system.”
A ‘digital twin’ for diabetes control
While automated insulin delivery systems like the artificial pancreas help users better manage Type 1 diabetes, adaptive biobehavioral control technology is designed to improve blood-sugar control during the day, when fluctuations occur more frequently due to meals and physical activity.